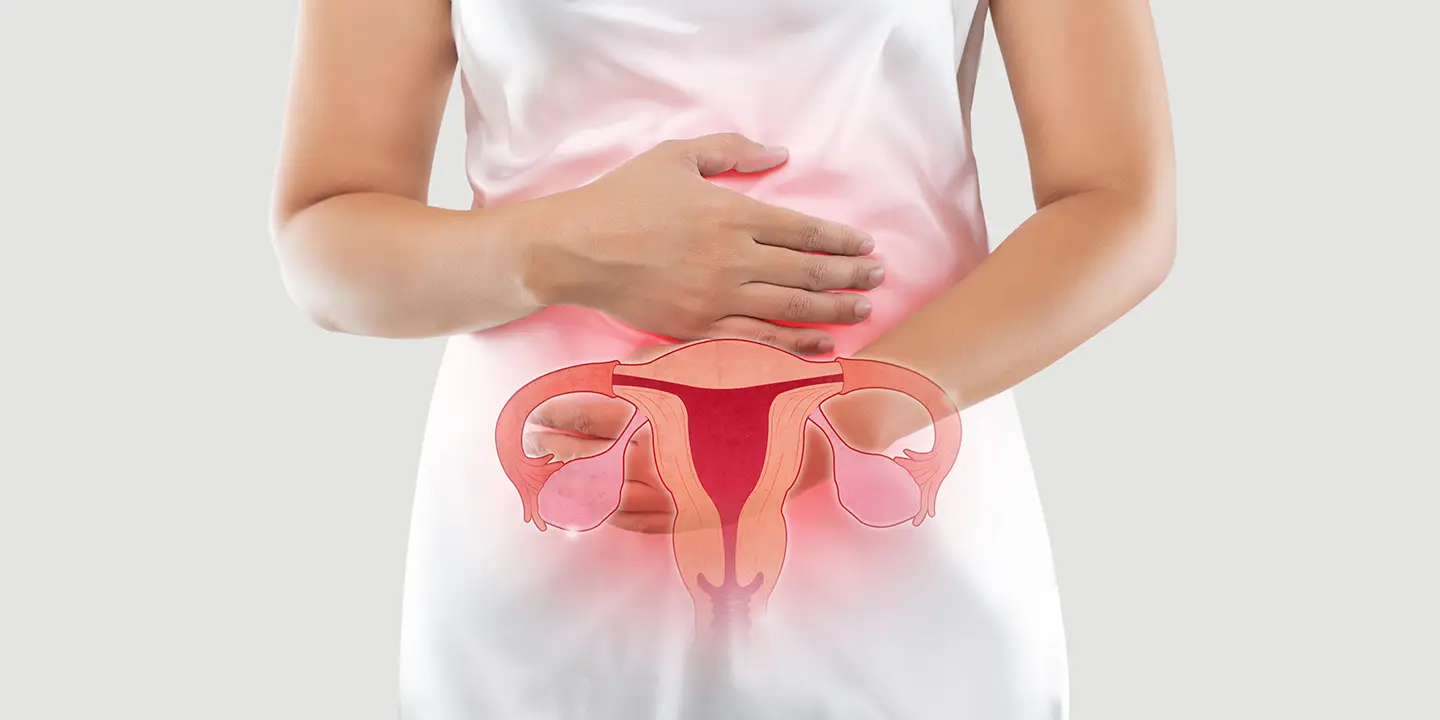
Pelvic pain during pregnancy is to be expected. After all, your ligaments are stretching, your hormone levels are fluctuating, and your organs are adjusting to accommodate your expanding uterus. However, discomfort can occasionally be a warning sign that something more serious is going on. Pelvic pain meaning is that your body is adjusting to physical changes in the belly and pelvis during pregnancy, or it could be Braxton Hicks contractions. Because causes of pelvic pain also include an ovarian cyst, infection, or early labor, you should always notify your healthcare physician.
The reasons for pelvic pain during pregnancy are discussed in this article. You’ll also discover why it’s critical to consult your doctor if you’re experiencing pain in your pelvic region or as the condition is commonly called pelvic pain pregnancy.
In this Article
1. Diastasis Recti
There may be a noticeable bulge in the middle of your abdomen during pregnancy. During pregnancy, the two sides of your rectus abdominus—the muscles that run from the top to the bottom of your abdomen—can stretch apart and split, resulting in diastasis recti (DR). Weakness might result from abdominal muscle separation. You may have difficulty carrying large objects. DR is common in the late second and third trimesters, and it might last following pregnancy. Though diastasis recti are not harmful, they can lead to problems. Medical attention may be required for side effects such as:
Bladder or bowel control problems
Weakness or pain that disrupts your everyday life
Consult your doctor if you are experiencing back pain during pregnancy or significant weakness.
Related Blog – 12 Week Of Pregnant Do And Don’ts For Healthy Delivery
2. Braxton Hicks Contractions
Braxton Hicks contractions are sometimes known as false labor pains since they feel like real contractions but do not indicate that you are in labor. Braxton Hicks contractions can happen as early as six weeks of pregnancy, but you won’t feel them. You may begin to have false labor pains in your second or third trimester, which can be alarming if your due date is still several weeks away. Braxton Hicks contractions are typical and are thought to prepare your body for the actual birth. What you’re feeling is your uterine muscle fibers tightening and relaxing.
Timing and regularity are two primary differences between true labor contractions and Braxton Hicks. Braxton Hicks contractions can commonly occur after having sex, being parched, or having a full bladder. Real labor contractions begin and end at regular intervals, becoming stronger and more painful as they progress.
Braxton Hicks contractions occur unpredictably and cause less discomfort. True labor contractions result in the delivery of the baby, whereas Braxton Hicks contractions do not.
If you are having contractions and are unsure if they are Braxton Hicks contractions, consult your doctor. You may be in labor if your contractions are regular, growing increasingly painful, or do not stop.
Seek medical treatment if you are experiencing any of the following symptoms in addition to your contractions:
- Bleeding or spotting
- The fluid is leaking.
- Unusual discharge, such as red or watery discharge
- Cramping or pressure in your abdomen
- Have a persistent dull back pain during pregnancy
These signs may indicate that you are in labor. If you are not yet 37 weeks pregnant, you may be in preterm labor and should visit a doctor as soon as possible. Don’t be concerned if it’s a false alarm; it’s always preferable to be certain, as practitioners see it all the time.
3. Vaginal Infection
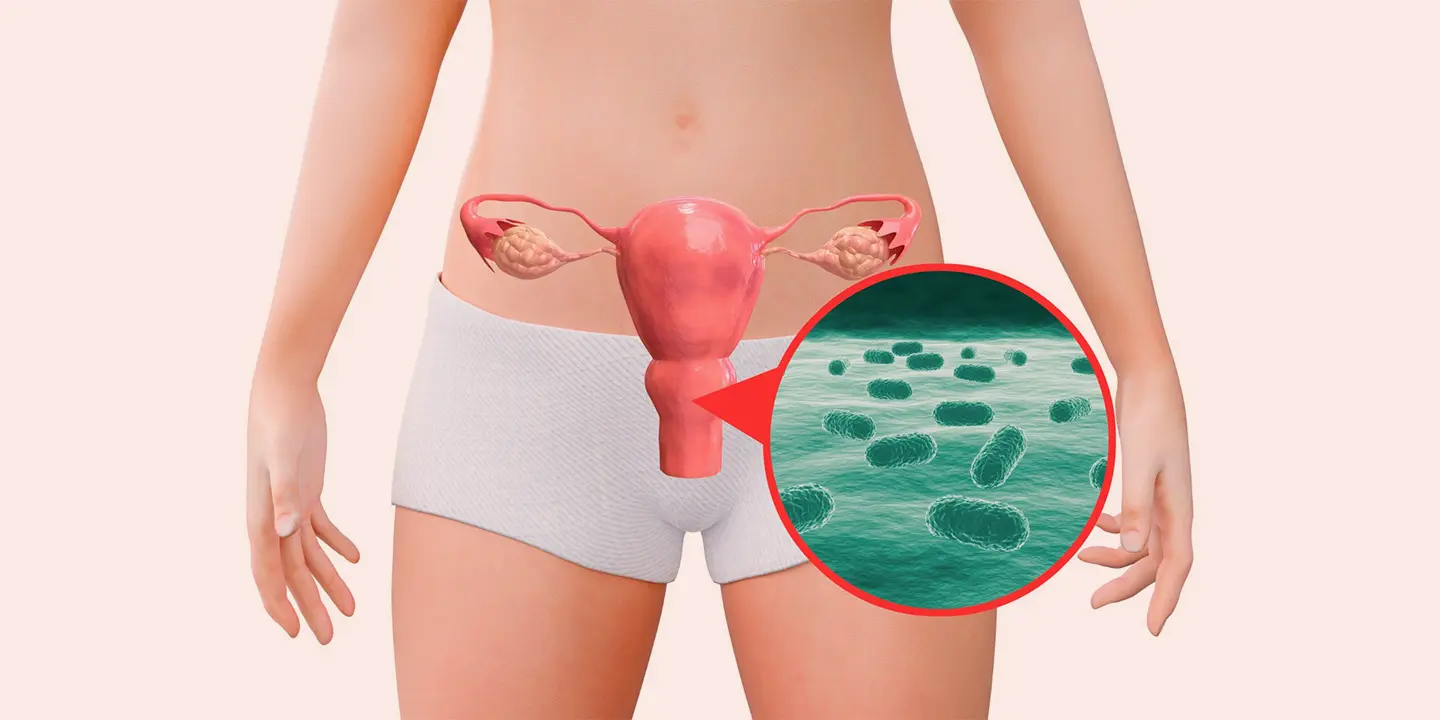
Vaginal infections can arise during pregnancy because altering hormones, particularly increased estrogen, upset your vagina’s usual acid balance. Yeast and bacterial vaginosis are two forms of vaginal infections that can cause a condition known as pelvic pain pregnancy.
Vaginal infections can cause itching, burning, redness, swelling, and pain around the vulva, which is located just outside your vagina. Pain can occur during sex or during urinating. You may notice spotting and changes in your discharge, such as an unexpected color, odor, or volume.
If your discharge is thin and milky, and you have no other pregnancy symptoms, it is most likely a pregnancy-related increase in discharge.
It could be yeast because it is white, has lumps, and is thick.
Bacterial vaginosis can be identified by foul-smelling or yellowish discharge.
Vaginal infections can occur at any stage of pregnancy. Consult your physician before using any medications, including over-the-counter therapies.
You should see your doctor if:
- Fever (temperature reaching 100.4 degrees Fahrenheit)
- Chills
- Pelvic discomfort
Related Blog : 10 Simple Ways To Prepare Your Body For First And Normal Delivery
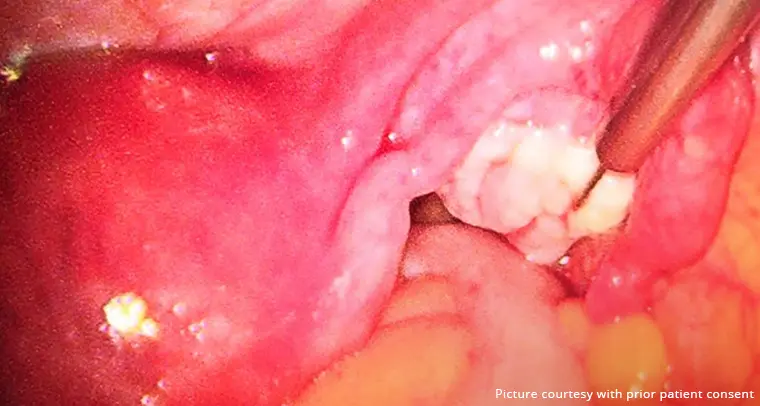
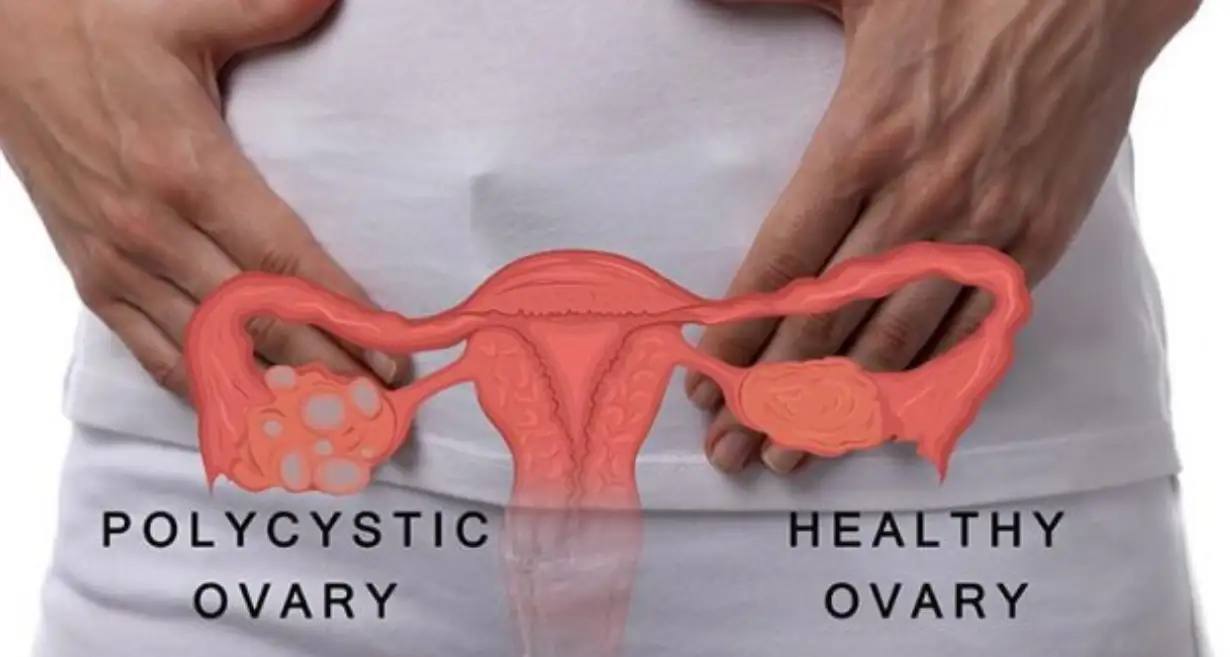
4. Ovarian Cyst
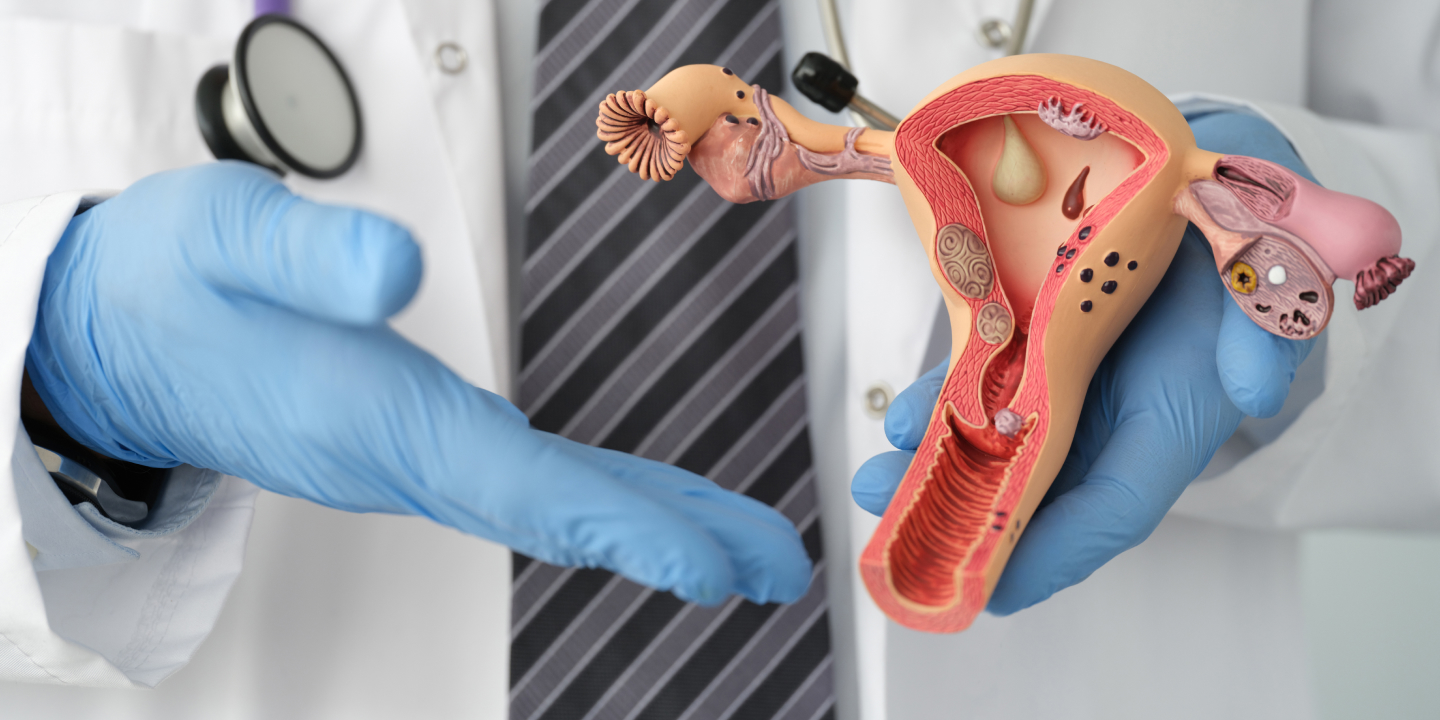
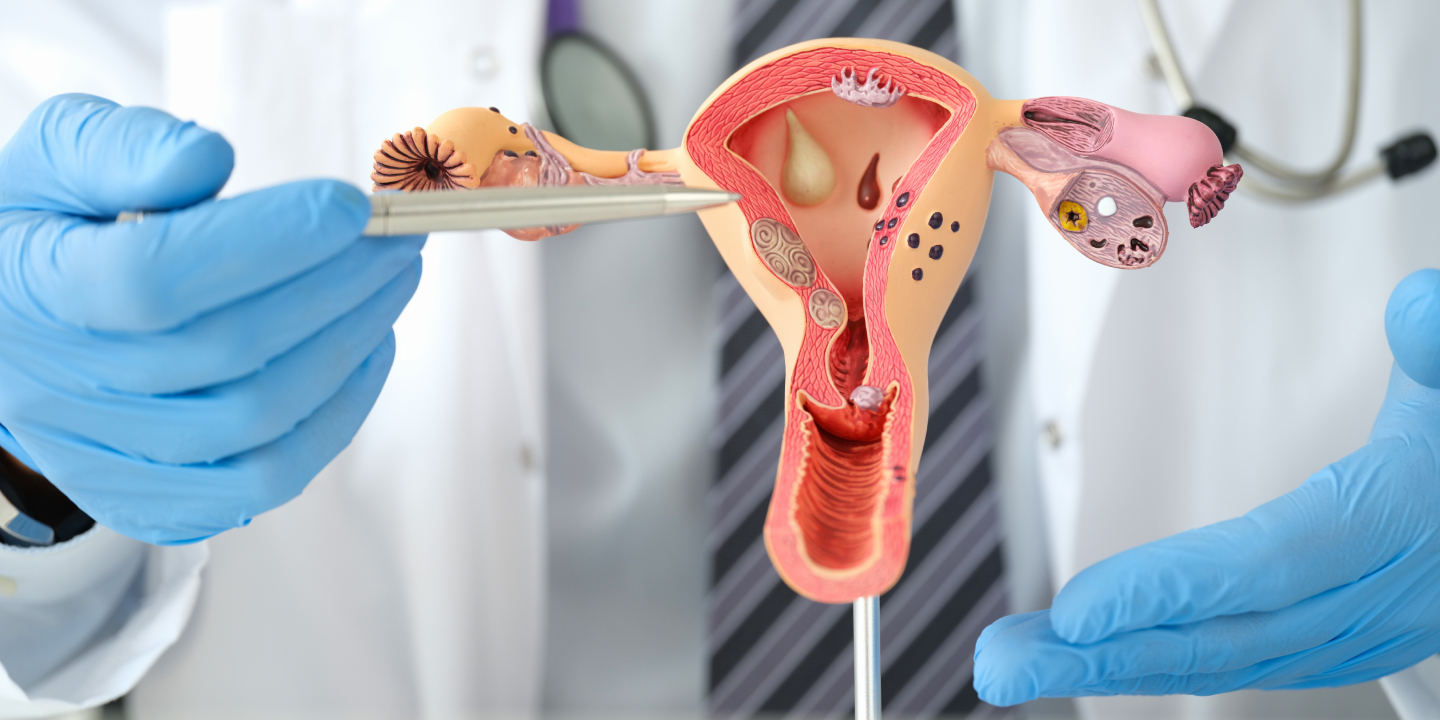
Ovarian cysts are tiny fluid-filled sacs that can form on or inside your ovaries. Two tiny oval-shaped ovaries are normally found in the lower abdomen. Every month, one of them will lay an egg. The ovaries are responsible for the production of the hormones estrogen and progesterone, which are involved in pregnancy. Ovarian cysts can appear at any time and go unrecognized most of the time.
Pelvic pain during pregnancy could also be due to a cyst during the first trimester. It normally does not cause any symptoms and typically goes away on its own.
A cyst that ruptures or twists might cause pain, bloating, or swelling on one side of your abdomen. The discomfort may be intermittent, dull, or acute, and stabbing. If you experience any pregnancy symptoms of an ovarian cyst throughout your pregnancy, you should consult your doctor. If you are in your first trimester, the symptoms could be a warning of a more severe scenario, such as an ectopic pregnancy.
Seek emergency assistance if you have any of the following symptoms of an ovarian cyst:
- A sudden pain that is intense
- nauseousness or vomiting
- Bleeding in the vagina
- dull backache
- Emptying your bladder or bowels is troublesome
- Feeling the urge to pee frequently
- Feeling dizzy or faint
- Fever (temperature reaching 100.4 degrees Fahrenheit)
5. Round Ligament Pain
Pain in the round ligaments is common during pregnancy. The circular ligaments resemble ropes or cables and connect your uterus to your groin. These ligaments support your uterus and may become painful during the second trimester as they soften and stretch to accommodate your growing tummy.
If you have round ligament pain:
You may feel as if something is pushing on your insides.
It could be abrupt and sharp.
Pain is felt on the right side of your abdomen, although it can also occur on the left or both sides.
Sudden movements, such as rolling in bed, can set off the discomfort. Often, sitting or lying down and resting will relieve the pain. If unexpected movements cause you pain, try to avoid them.
While round ligament discomfort is not harmful, you should report it to your doctor. Consult your doctor if:
- When you pee, you feel pain.
- Bleeding
- Vomiting, nausea, or bloating
- Fever (100.4 degrees Fahrenheit) or chills, which could indicate an infection
- Excruciating pain
- Spreading pain to your back
- Having difficulty walking
6. SIJ Pain (Sacroiliac Joint)
SIJ pain is a type of low back pain during pregnancy that can spread down your legs. The bones that make up your pelvic girdle are located at the base of your spine, around your pelvis. The pelvic girdle is supported by the two sacroiliac joints, which are placed at the back of your body. Weight increase may also cause the condition of pelvic pain pregnancy as there is a strain on your pelvic girdle bones and joints. Your joints may begin to bear the weight unevenly, putting more strain and friction on your SIJ.
SIJ pain usually begins in the late second or third trimester. Hormonal changes during pregnancy are another issue. The same hormone that relaxes your muscles and prepares them for delivery can damage the ligaments that provide support, resulting in pain.
When ascending stairs, walking, rolling over in bed, balancing, or getting out of the bathtub, you may experience pain. SIJ discomfort can be felt in the lower back, the legs, or the hips and groin. This pain might be acute or dull and numbing, making you feel as if your leg is about to buckle. If your back pain during pregnancy is severe or does not go away no matter what posture you are in, consult your doctor.
Medical treatment is required for the following pregnancy symptoms of SIJ:
- Bleeding in the cervix
- Fever (temperature reaching 100.4 degrees Fahrenheit) (temperature reaching 100.4 degrees Fahrenheit)
- When you pee, there’s a burning sensation.
Related Blog : Am I Pregnant? 10 Early Pregnancy Signs and Symptoms
7. Symphysis Pubis Dysfunction (SPD)
SPD is sometimes known as pelvic girdle pain because, like SIJ pain, it affects the pelvis—in this case, the front of the pelvis.
SPD reasons are the same as SIJ—relaxin and weight increase, which generate uneven pressure and friction on the bones and joints of the pelvic girdle.
SPD discomfort is characterized by shooting pelvic pain meaning, at the front of the pelvis that may spread to the lower abdomen, back, groin, perineum, and thighs. You may hear or feel clicking, grinding, or snapping sounds. It may worsen when you climb stairs, get in and out of bed or the bathtub, or bend over.
You should notify your healthcare physician if you are experiencing pelvic girdle pain, especially if you are having difficulty moving or if going up and down stairs is bothersome. If you have any other symptoms, it could indicate that something more serious is wrong.
Seek emergency medical attention if you have:
- Bleeding in the cervix
- Fever (temperature reaching 100.4 degrees Fahrenheit) (temperature reaching 100.4 degrees Fahrenheit)
- Burning sensation while urinating
8. Pubic Symphysis Separation
The pubic symphysis is a joint that connects the bones in your pelvis. This joint has to broaden during pregnancy to allow for delivery. This expansion can sometimes produce pain as the pelvis becomes unstable and less supportive.
Pubic symphysis separation, also known as diastasis symphysis pubis (DSP), is characterized by shooting, and intense pain in the front of the pelvis. The discomfort may radiate to your lower back, hips, thighs, lower abdomen, and the back of your legs. A clicking, grinding, or snapping sensation is possible.
When you shift over in bed or carry your infant on one hip, the pain may worsen. If you walk with a waddle, it could be due to pubic symphysis separation.
This problem can, in certain situations, prevent you from completely emptying your bladder, which can lead to urinary tract infections.
The following are indications that something else is going on that requires immediate attention:
- Bleeding in the cervix
- Fever (temperature reaching 100.4 degrees Fahrenheit)
- Leg sluggishness or discomfort
- Headache
- bladder or bowel control problems
9. Miscarriage
Miscarriage is a loss of a pregnancy that occurs before the 20th week. Most occur early in the pregnancy, sometimes before the woman is aware of the pregnancy, and frequently go unrecognized. Miscarriage occurs in 10 to 20% of known pregnancies. Although pregnancy loss is frequent, it can be emotionally draining.
Miscarriage cannot be stopped once it has begun. If the embryo or fetus is not developing normally, miscarriage can occur.
Although miscarriage cannot be prevented, it is critical that you consult your healthcare practitioner. Miscarriage can result in severe bleeding or infections. Getting counseling done with respect to the emotional component of pregnancy loss is also beneficial for many people who go through it.
Among the warning signs are the following:
- Your vaginal bleeding or spotting
- Cramping or discomfort in your lower abdomen, shoulder, or low back
- Clots, fluid, or tissue going through your vagina
- Pain while using the restroom
- Dizziness or fainting
- Fever (high temperature of 100.4 degrees Fahrenheit) or chills
Not every early pregnancy bleeding is a miscarriage. Mild spotting during the first trimester of pregnancy is usually harmless. However, you should notify your healthcare physician.
Related Blog : 11 Tips for a Safe, Healthy Pregnancy
10. Preterm Labor
Pelvic pain meaning is that you could also be in preterm labor. Preterm labor occurs when contractions and cervical opening for birth occur prematurely. Preterm labor can occur between the 20th and 37th week of pregnancy and affects approximately 12% of pregnancies.
You are considered full-term if you are 37 weeks or older. The earlier premature labor develops between the ages of 20 and 37 weeks, the more are the chances of it being risky it is.
If you believe you are in labor before 37 weeks of pregnancy, seek emergency medical treatment.
Preterm labor pregnancy symptoms include:
- Contractions, which feel like an abdominal tightening
- Low backache that is dull and persistent
- Cramping or abdominal pressure
- spotting or vaginal bleeding
- Your vaginal fluid has gushed out.
- a mucus-like or bloody discharge
Frequently Asked Questions
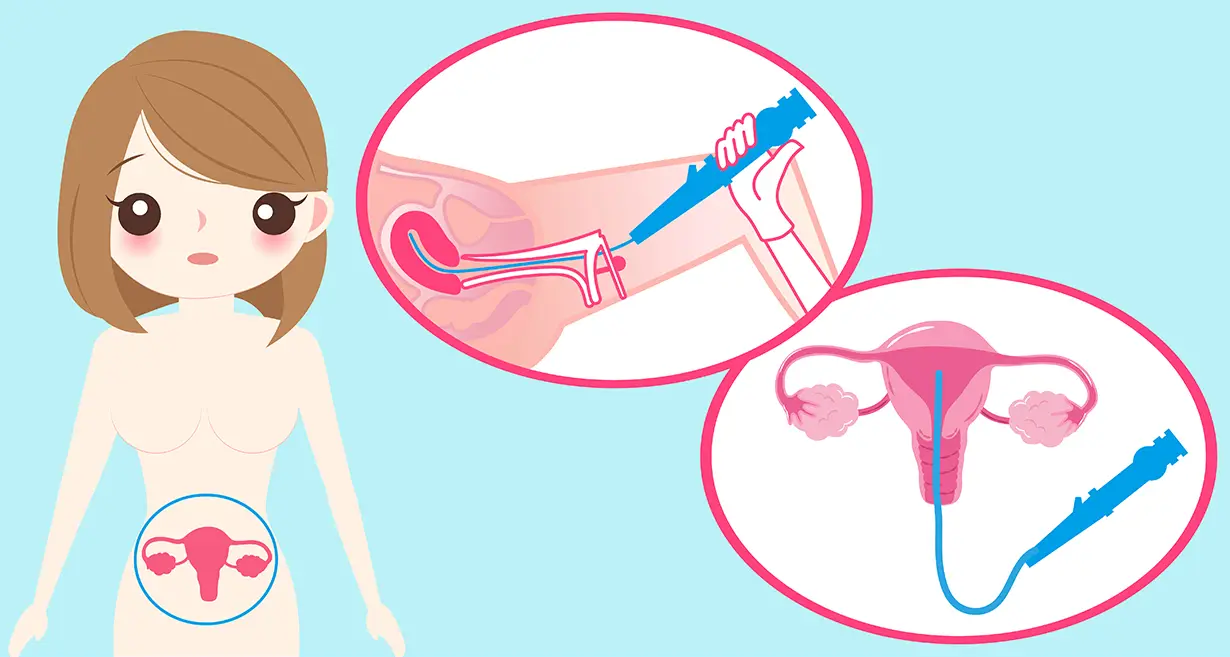
Pelvic pain during pregnancy can be caused by a variety of factors, so your physician will need to check you carefully to establish what is causing it. Your practitioner may inquire about your activities and habits, such as whether you’ve used drugs or been in an accident.
Inform your doctor of any pregnancy symptoms you are experiencing, even if they are humiliating or appear to be unconnected to the pain. Your vagina and cervix may be examined by your doctor. A pelvic examination is most likely. You may be subjected to blood tests and an ultrasound.
You are more prone to experience pelvic pain if you:
• Experienced pelvic pain during a previous pregnancy.
• Have had several pregnancies.
• You have a history of pelvic trauma, such as a back injury or a pelvic fracture.
• Engage in difficult exercises including lifting, twisting, and bending.
Being overweight or carrying a large baby (a condition known as macrosomia) may also increase your risk of pelvic pain, but the data is mixed.
Pelvic pain in the first trimester is typically caused by your body changing to and accommodating the baby. It could also be linked to digestive problems that worsen during pregnancy, such as gastroesophageal reflux disease (GERD). Miscarriage can also induce pelvic pain in early pregnancy. An ectopic pregnancy, or pregnancy that happens outside the uterus, is the most dangerous cause of pelvic pain in early pregnancy. Ectopic pregnancies necessitate prompt medical treatment.
Conclusion
Pelvic pain during pregnancy can be frightening. It is reasonable to be concerned, and discussing your pain with your healthcare doctor is a good idea. Most causes of pelvic pain are not serious, but it might signify an emergency in some cases. If you are experiencing severe or unusual pain, bleeding, fever, chills, or other troubling symptoms, it’s crucial to talk to your doctor or OB-GYN.
Good prenatal care is critical for not only your baby’s proper development but for a pain-free and healthy pregnancy for the mother as well. It also helps to have an excellent team of obstetricians and gynecologists on your side, which is what you receive at Queen’s Gynecology in Delhi. The highly trained and skilled team of doctors at Queen’s Gynecology will not only help to soothe your concerns about your symptoms but will also offer you world-class treatment so that you may continue to have a pain-free and joyous pregnancy journey. Queen’s Gynecology’s superb team of obstetricians and gynecologists believes in treating their patients with the highest compassion and humanistic touch. After all, there’s a queen in every woman!