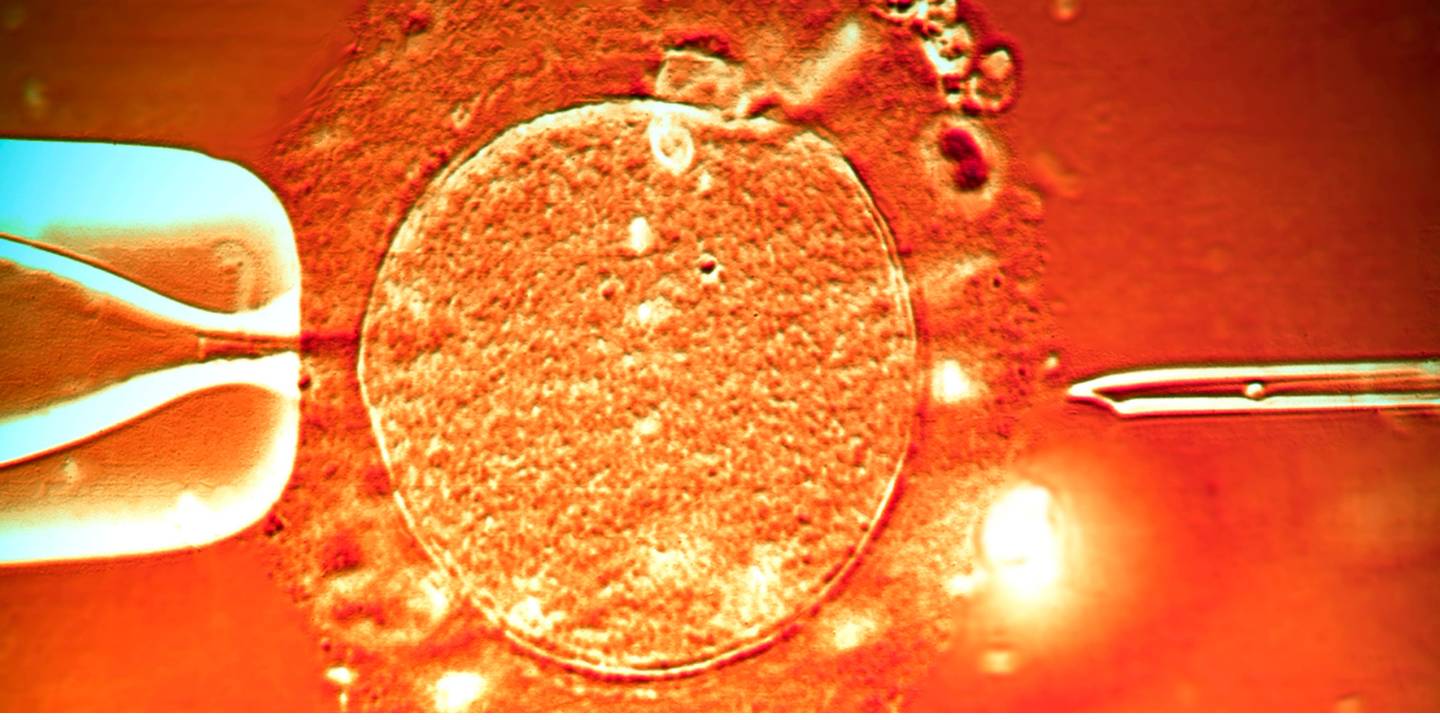
Starting the IVF process is like solving a challenging problem piece by piece. It has great potential, yet occasionally you could find yourself with missing elements. In vitro fertilisation, or IVF, is a source of optimism for prospective parents, but what if it fails to work?
IVF is a crucial component of fertility treatments, but when it fails, the emotional toll along with the financial burden may be debilitating. Anyone who sets out on this path must comprehend its causes. In this article, we’ll examine the top 10 causes of IVF failures, ranging from poor egg quality to uterine concerns. We hope to educate and encourage people who are dealing with the complex process of reproductive treatments by outlining these difficulties. Keep in mind that you are not alone and that there is still hope despite obstacles.
Related Blog: Female Infertility – Causes, Symptoms, Diagnosis and Treatments
In this Article
Top 10 Causes of IVF Failure
IVF failure may be emotionally taxing, therefore it’s important to comprehend its causes.
- Embryo Quality: The quality of the embryos is one of the most important aspects of IVF success. Embryos are assigned grades depending on how they seem and how well they could develop. Poorly made embryos might prevent implantation or cause an early miscarriage. Issues with embryo quality can result from things like chromosomal defects, uneven cell division, and even the thawing and freezing procedure in frozen embryo transfers. Preimplantation genetic testing (PGT-A), a thorough genetic test, can help find chromosomal problems prior to embryo transfer, improving the likelihood of choosing a healthy embryo.
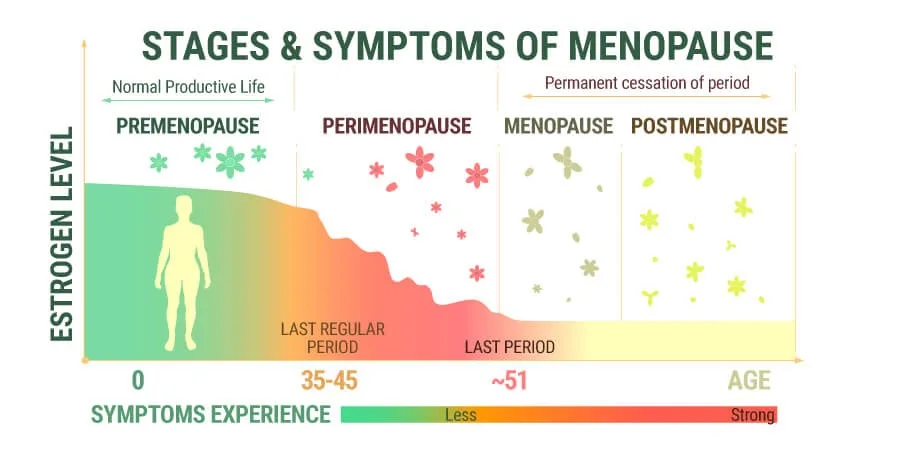
- Age: The success rates of IVF are strongly impacted by a woman’s age. It is more difficult to have a successful pregnancy at advanced maternal age, which is commonly classified as above 35, because the number, as well as the quality of eggs, are linked to a reduction. Because their eggs tend to be healthier on average, younger women are likely to have greater pregnancy rates. The likelihood of success for women older than 35 is lower every year. Over 40 women frequently confront even more difficult circumstances, which might involve a higher chance of miscarriage and embryonic chromosomal abnormalities.
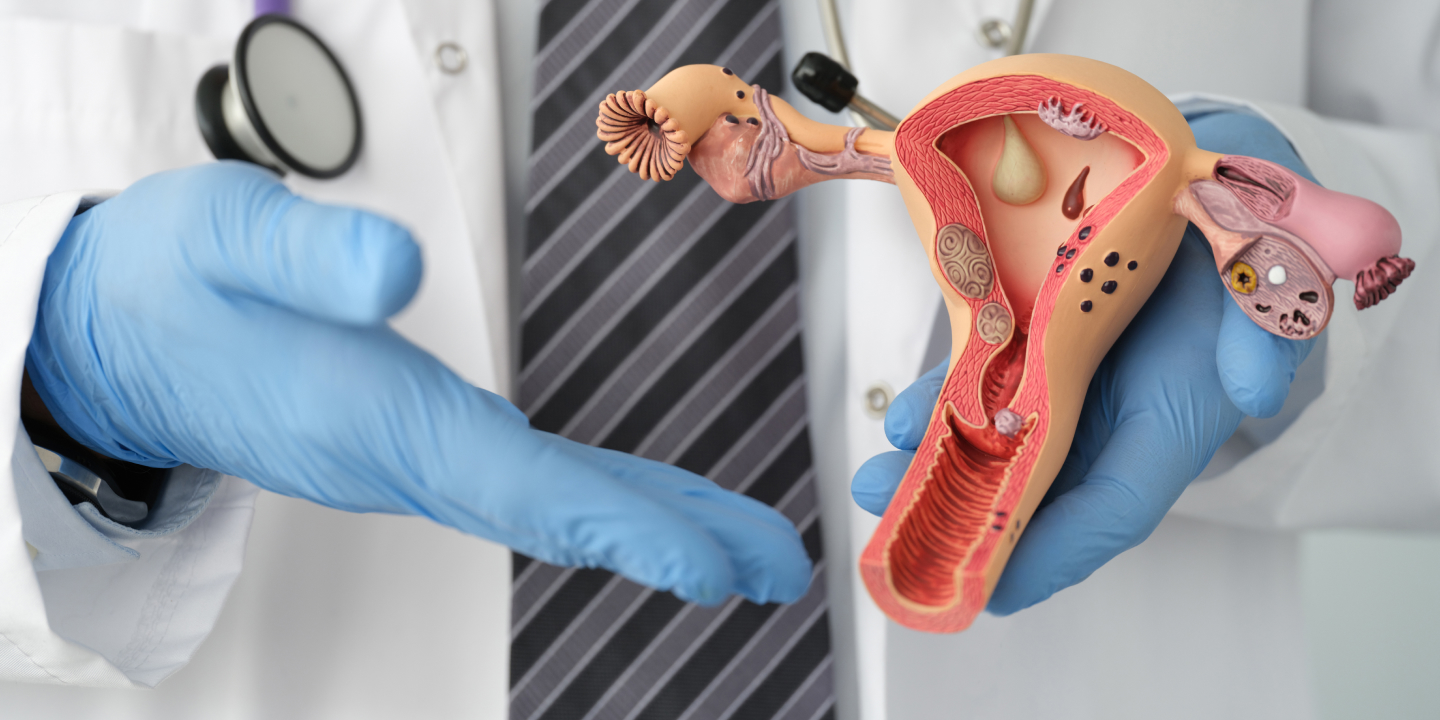
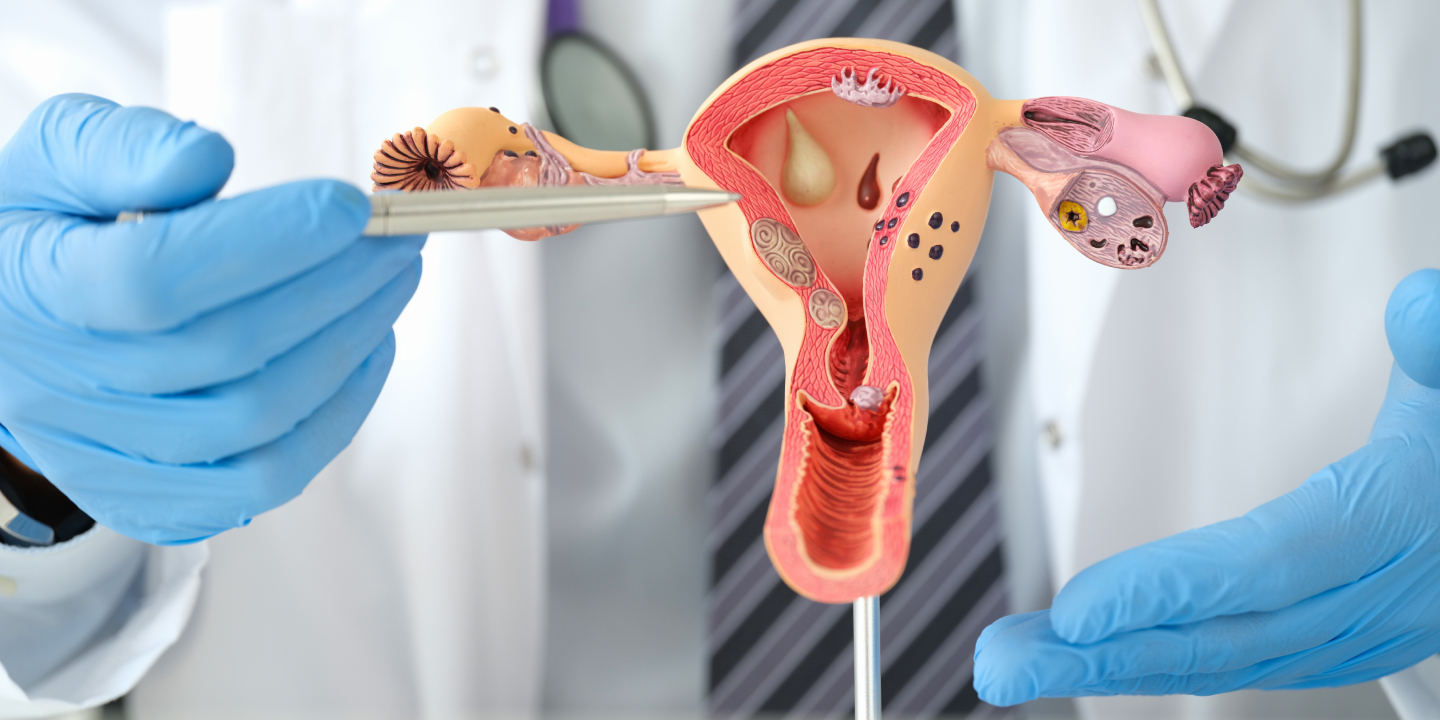
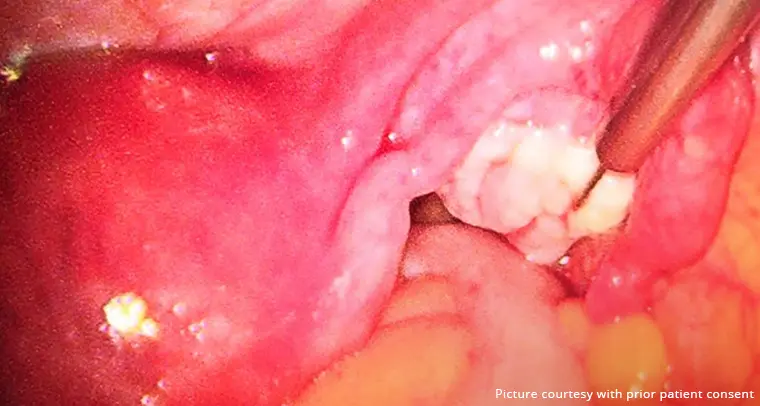
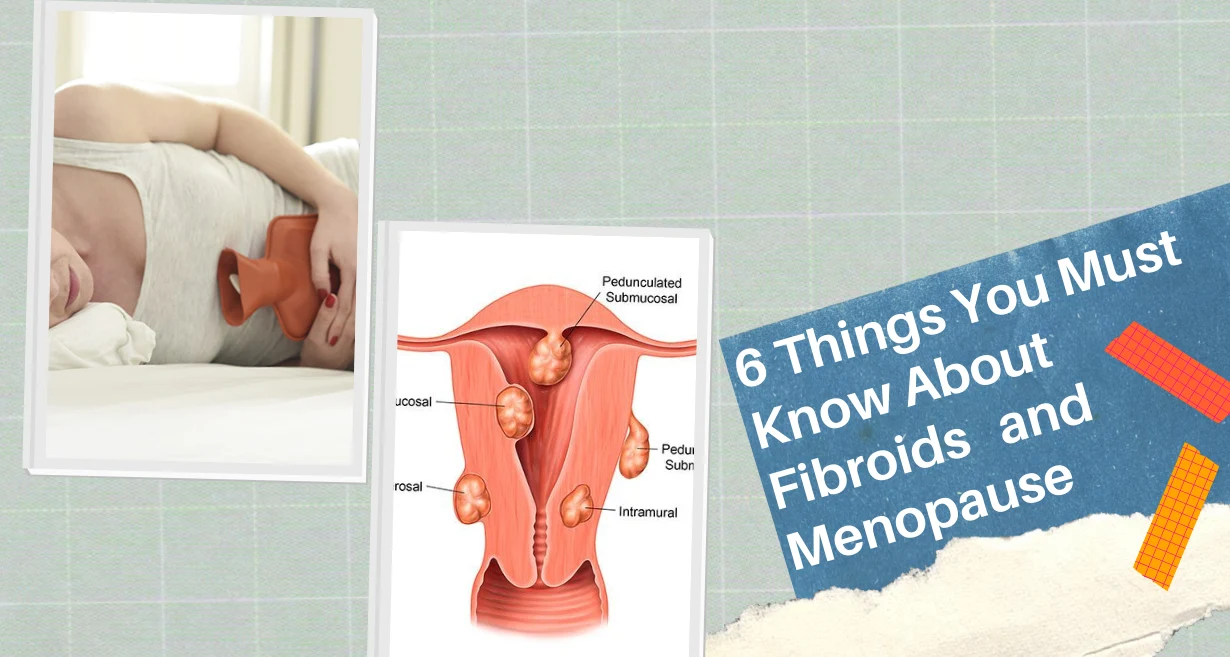
- Uterine Issues: The uterus itself may have issues that prevent embryo implantation. Issues like fibroids or polyps may impede the embryo’s ability to connect to the uterine lining or possibly produce an unfavourable environment for implantation. Before starting IVF, uterine anomalies might need to be surgically corrected. These problems can be addressed by procedures like hysteroscopy, potentially increasing the likelihood of pregnancy success.
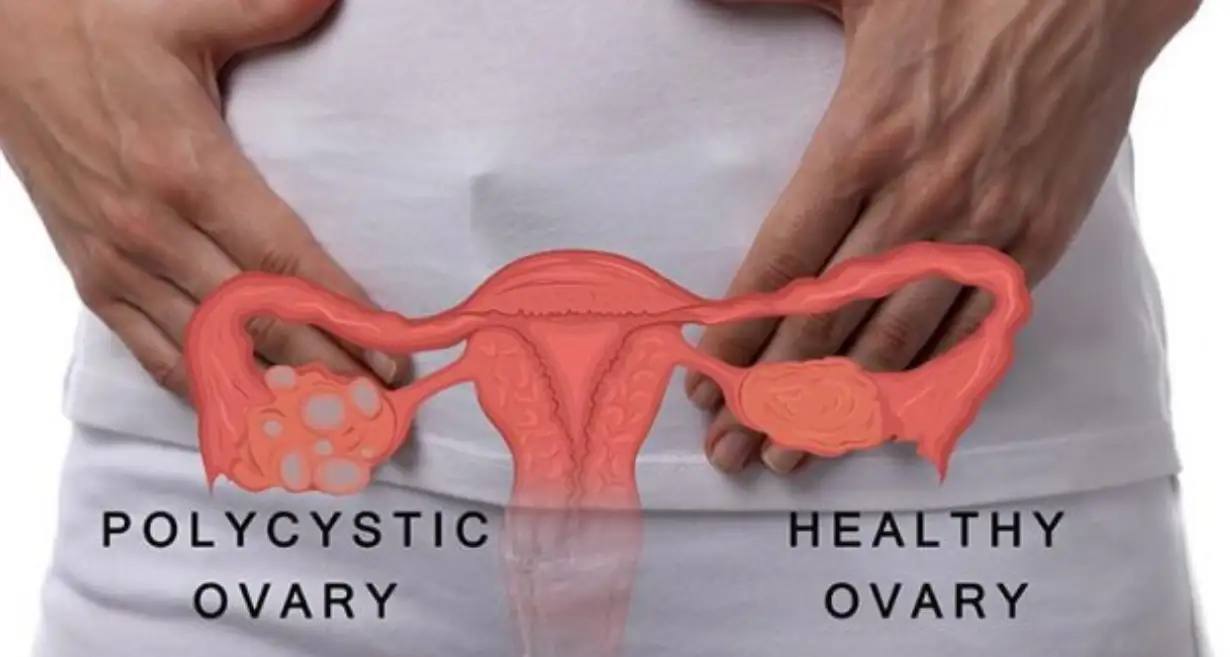
- Ovarian Issues: The ovaries are essential to IVF. Ovarian hyperstimulation syndrome (OHSS), which affects IVF results, can develop from an overactive reaction to fertility medicines, while an inadequate response might lead to too few eggs being recovered. A significant aspect is ovarian reserve, which describes the amount and calibre of a woman’s eggs. Fewer eggs may be produced by women who have less ovarian reserve, which would reduce the quantity of embryos ready for transfer. On the other side, ovarian hyperstimulation syndrome can cause major medical issues and lower the likelihood of embryo implantation.
- Quality of Sperm: The quality of the sperm is of critical significance when it comes to fertility treatments. Poor Motility and low sperm count that is low, are known as poor sperm quality which may obstruct fertilisation and development of an embryo. DNA fragmentation analysis, and Intracytoplasmic sperm injection (ICSI), may be used in situations of severe infertility in males.
- Genetics: The biological traits of each spouse can have an influence on the embryo’s health. Chromosomal difficulties can be caused by genetic problems that may affect the sperm or the egg, making it difficult for an embryo to take root or raising the chance of miscarriage. There are ways available, like genetic testing, to detect these abnormalities in embryos prior to they are transplanted. The genetic testing like PGT can increase the likelihood of choosing viable eggs, which is particularly critical if there is an indication of genetic issues or frequent losses.
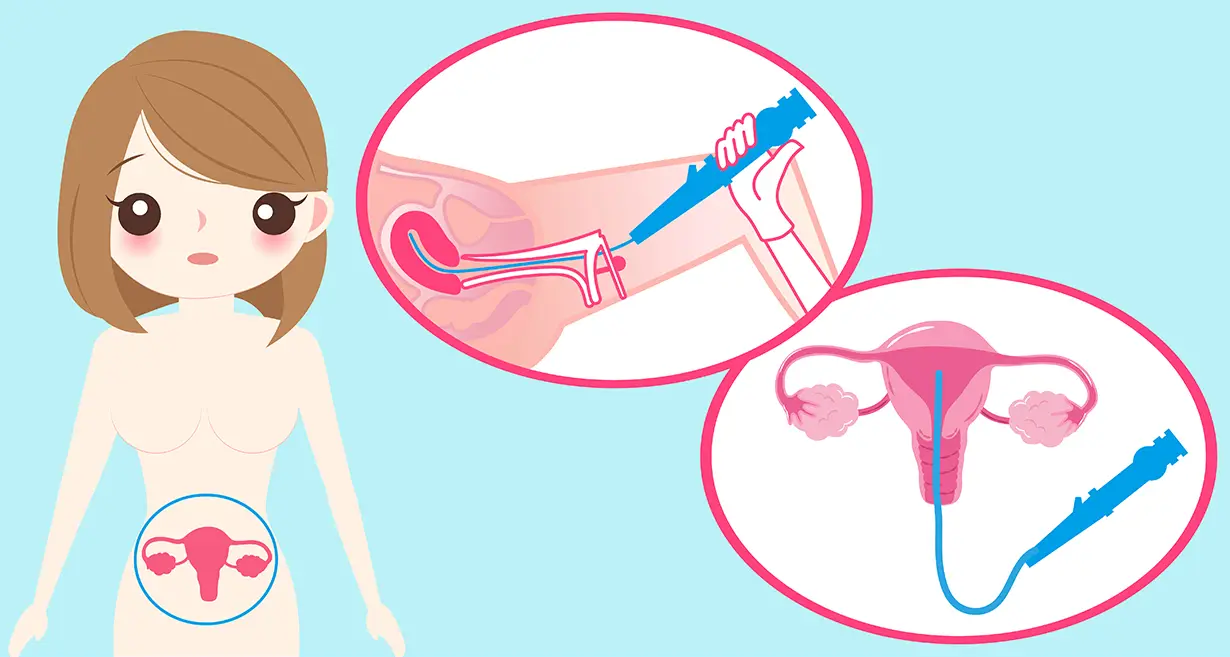
- Implantation Failure: The embryo may not always adequately connect to the lining of the uterus. Problems with the embryo or within the environment of the uterus may cause this to happen. The endometrium, the lining of the uterus, must be sufficiently ready to accept the embryo. Implantation failure can be caused by things like hormone imbalances, inadequate thickness of the endometrium, or some immunological factors. Hormonal remedies and procedures including IUI (intrauterine insemination) might be taken into consideration to address these problems and increase the likelihood of implantation to be a success.
- Endometriosis: In this disorder, tissue that resembles the uterine lining grows out of the uterus. It could have an impact on the effectiveness of IVF and fertility since it might cause swelling and scarring. Endometriosis patients may have a diminished ovarian reserve, poorer-quality eggs, and a greater chance of failed implantation. Laparoscopy surgical treatment that eliminates endometriotic tissue, may be advantageous for certain people.
- Anxiety and stress: These factors might affect the outcome of IVF. It’s crucial to control stress amid fertility treatments since it may disrupt the hormonal equilibrium and uterine blood flow. Practising meditation, yoga, and acupuncture are examples of mind-body techniques that might lessen stress. Along the way of IVF, getting support from a counsellor or joining a peer group may be quite helpful emotionally.
- Lifestyle Factors: Lifestyle considerations are important. Obesity, heavy drinking, and smoking can all have a detrimental impact on IVF results. The likelihood of success can be increased by leading a healthy lifestyle. Particularly smoking has a negative effect on conception and IVF success. It has been linked to lower ovarian reserve, an increased likelihood of having an ectopic pregnancy, and increased miscarriage rates. It is very advised to stop smoking before beginning IVF to maximise results.
Managing IVF Failure
Failure during IVF may be emotionally draining. Here are some practical tips for handling IVF failure:
- Ask friends, relatives, or a therapist with experience in reproductive difficulties for emotional support.
- Keep in mind that you’re not alone and that talking about your feelings might help you feel better.
- Take a pause to allow your body and mind to recover. Consider your path.
- When you’re ready, take into account alternate routes like adoption or donation alternatives.
- Adopt a healthy lifestyle by emphasising self-care through your favourite hobbies.
- Maintain a cheerful outlook and be open to what the future may bring.
Related Blog: First Pregnancy Scan After IVF (In Vitro Fertilization) Treatment
Conclusion
Keep in mind that while these difficulties are genuine, they can be overcome as you work with your gynecologist to grasp the main reasons why IVF treatments fail. The most important thing is to persevere, and getting expert advice is crucial. At Queen’s Gynaecology, we provide cutting-edge therapies for problems relating to infertility that are suited to your particular needs. For conditions like removing endometriotic lesions, uterine fibroids, ovarian cysts, polyps, and adhesions as well as the management of tubal pathologies, uterine and pelvic anomalies, and congenital disorders of the reproductive tract, our comprehensive care includes emotional support, thorough diagnostics, and individualised solutions.
From start to finish of your journey, we make sure you get attentive, individualised treatment. If you’ve encountered obstacles, don’t give up; you may still take the steps necessary to become a parent. You can manage these difficulties and improve your chances of having a successful IVF experience with the appropriate help and knowledge.
FAQ’s
Failure of the implantation of the embryo is the most frequent cause of IVF (In Vitro Fertilisation) failure. Even after being implanted into the uterus, even an excellent quality embryo may not survive. It occurs for a number of reasons, including problems in the lining of the uterus, poor-quality embryos, or those that are unable to connect to the inside of the uterine wall.
Even if high-quality embryos are transferred, IVF might still fail. Due to concerns with the condition of the uterus, genetic anomalies with the embryo, or problems with the embryo’s capacity to adhere correctly to the lining of the uterus, even the highest-quality embryos may not implant. Sometimes, undiagnosed medical issues in either spouse might have an effect on the effectiveness of IVF.
Age-related variables, physical disorders, lifestyle habits, and unidentified infertility are just a few of the many potential causes of IVF failure in some people. Age is a crucial consideration since fertility decreases with age, making IVF pregnancy more challenging. Additionally, medical issues such as endometriosis or polycystic ovarian syndrome (PCOS) might hinder the outcome of IVF.
Though IVF may have established itself as an effective and cutting-edge fertility procedure, it isn’t always successful. The likelihood of success varies depending on several variables, like age, the couple’s health, and their unique situations. Even with the best professional care given medically, there is no assurance that fertility treatments will always be successful.
Is the second cycle of IVF more successful?
IVF success rates might change from cycle to cycle. Some couples could experience success after the first cycle, and some might need more than one. The reason for infertility and the changes to your plan of treatment by your doctors, in light of prior cycles are two key factors that affect whether the second IVF round is successful. It’s crucial to speak with an IVF expert to decide the best course of action for your particular circumstances and raise your chances of conceiving successfully.