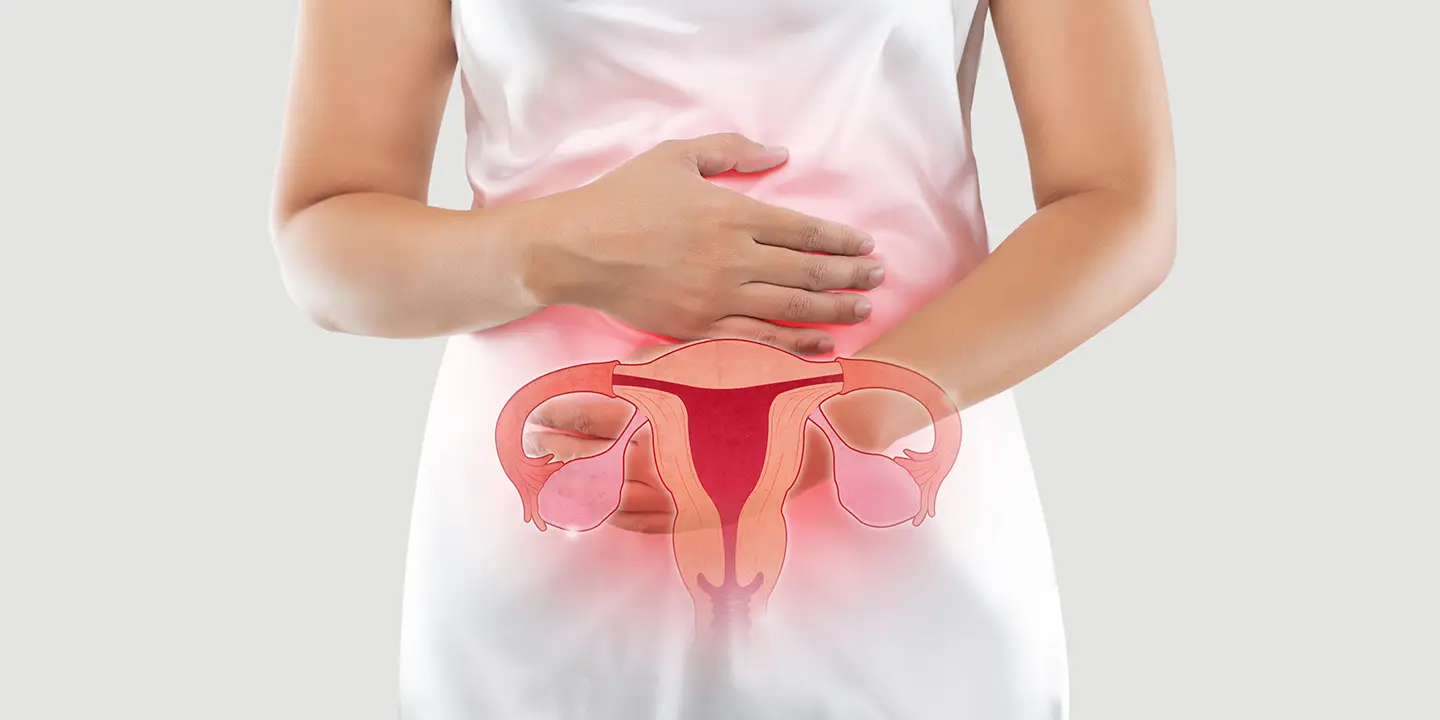
Women frequently worry about menstruation problems, which are commonly associated with symptoms such as abnormal or irregular menstrual cycle patterns. Due to the discomfort, anguish, and emotional distress, they can cause, these conditions can drastically lower a woman’s quality of life. We’ll look at the many menstruation disorders, their causes, symptoms, diagnoses, and potential treatments in this blog post.
In this Article
Menstrual Disorders
A variety of conditions that can have an impact on a woman’s menstrual cycle are referred to as menstrual disorders. These conditions can result in anomalies in the timing, length, or flow of the menstrual cycle, which can be painful physically and upsetting emotionally.
Before your period, menstrual cycles frequently cause a number of painful sensations. Mild cramps, exhaustion, and other typical problems are all included in premenstrual syndrome (PMS), but the symptoms normally disappear or reduce in severity once your period starts.
Other women, however, due to an irregular menstrual cycle, experience a variety of physical and/or emotional symptoms right before and during menstruation. A woman’s life may be significantly disrupted by these symptoms, which can range from excessive bleeding and missing periods to uncontrollable mood swings requiring medical intervention.
Types of Menstrual Disorders
Different menstruation problems might have an impact on women. Let’s delve more into a few of the prevalent menstrual disease categories:
Amenorrhea
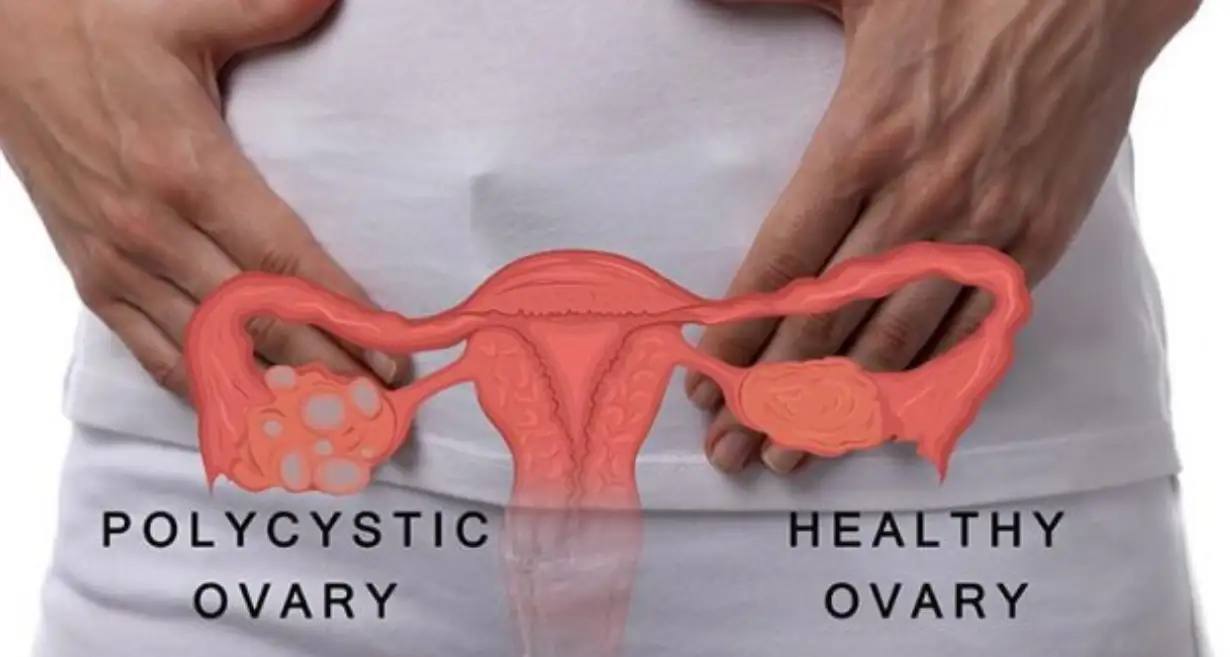
The lack of menstruation is known as amenorrhea. It is categorized as either primary or secondary. Secondary amenorrhea is the cessation of menstruation for more than three months in women who previously had regular cycles, whereas primary amenorrhea is the failure of menstruation to begin by the age of 16. Hormonal imbalances, polycystic ovarian syndrome (PCOS), thyroid conditions, excessive exercise, stress, and specific drugs are some of the common reasons for amenorrhea.
Dysmenorrhea
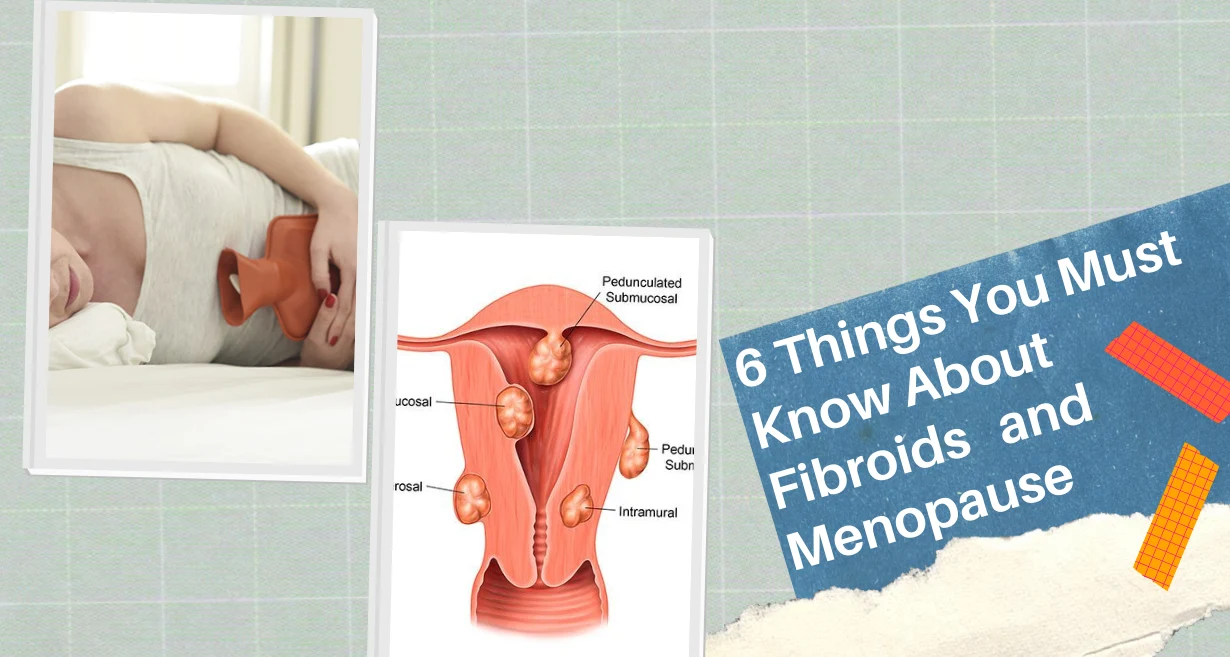
Dysmenorrhea refers to painful menstruation. It is categorized as either primary or secondary. Primary dysmenorrhea often starts in adolescence and is unrelated to any underlying medical conditions. It is brought on by elevated prostaglandin levels, which promote hard uterine contractions. Contrarily, diseases such as endometriosis, uterine fibroids, pelvic inflammatory disease (PID), or adenomyosis are responsible for secondary dysmenorrhea.
Menorrhagia
Menorrhagia is characterized by excessive or protracted menstrual bleeding. Menorrhagia can cause bleeding that lasts beyond seven days or necessitates frequent sanitary product changes in women. Hormonal imbalances, uterine fibroids, polyps, adenomyosis, endometrial hyperplasia, or specific bleeding diseases can all contribute to menorrhagia. It can cause anemia and have a very negative effect on a woman’s daily life.
Oligomenorrhea
Oligomenorrhea is the medical term for irregular or infrequent menstrual cycles that last longer than 35 days. It can be brought on by PCOS, thyroid issues, hormonal imbalances, stress, excessive exercise, severe weight changes, or premature ovarian failure. Planning a family may be difficult for women with oligomenorrhea since they may find it difficult to predict when their periods will come.
Premenstrual Syndrome (PMS)
PMS is a term used to describe a variety of emotional and physical symptoms that occur in the days before a period. Mood swings, bloating, breast soreness, exhaustion, and changes in appetite may be among these symptoms. Although the precise etiology of PMS is unknown, hormonal changes and neurotransmitter abnormalities are thought to have a role in its onset. The impact of symptoms on a woman’s ability to operate on a daily basis might range from modest to severe.
Premenstrual dysphoric disorder (PMDD)
PMDD is a serious form of premenstrual syndrome (PMS) marked by extreme mood swings, melancholy, irritability, anxiety, and other emotional symptoms. Compared to PMS, PMDD symptoms are more intense and incapacitating. A woman’s quality of life, relationships, and everyday activities can all be adversely impacted by PMDD. Hormonal and neurotransmitter imbalances, as well as genetic and environmental factors, may all contribute to PMDD, however, the specific etiology is unknown.
Symptoms Of Menstrual Disorders
Menstrual diseases can have a variety of symptoms, which further differ from person to person and depend on a particular ailment. The physical and emotional health of a woman may be greatly impacted by these symptoms, which can be moderate to severe. The following are some typical signs and symptoms of menstruation disorders:
- Periods that are irregular or nonexistent are common signs of numerous menstrual diseases. This can involve menstrual cycles that are either less frequent (oligomenorrhea) or more frequent (polymenorrhea). Menstrual irregularities, often known as amenorrhea, can occur in certain women.
- Menorrhagia, which is characterized by excessive or protracted menstrual flow, is a common sign of a number of menstrual problems. Menorrhagia can cause bleeding that lasts longer than seven days or necessitate frequent sanitary product changes in women.
- Dysmenorrhea, or unpleasant menstruation, is another typical symptom. It causes discomfort and cramps. Lower abdominal cramps in women with dysmenorrhea can range from minor discomfort to excruciating pain. The pain might affect everyday activities and may spread to the thighs or lower back.
- Mood swings and emotional shifts are common in women with menstruation problems. Among them include irritation, anxiety, depressive symptoms, mood fluctuations, and modifications in general emotional health.
- Some women may experience fatigue, weariness, or poor energy. This might be brought on by erratic hormone levels, heavy bleeding, or underlying illnesses.
- Migraines or headaches are frequent side effects connected to menstruation disorders. These headaches may be more severe for certain women and can happen before, during, or after menstruation.
- Before or during the menstrual cycle, women frequently suffer from bloating and breast soreness. Women may experience breast tenderness or pain as well as stomach swelling or discomfort.
- During their menstrual cycle, some women may notice changes in their appetite, including an increase in their appetites for particular foods. These cravings might be brought on by hormonal adjustments.
It’s crucial to remember that each person will experience symptoms differently, both in terms of severity and combination. It is advised to speak with a healthcare provider if you have any bothersome or recurrent symptoms connected to your menstrual period.
Causes Of Menstrual Disorders
The underlying causes of menstrual diseases might range from hormone imbalances to anatomical abnormalities. For these illnesses to be properly diagnosed and treated, it is imperative to comprehend the reasons. The following are some typical reasons for menstruation disorders:
Hormonal Imbalances
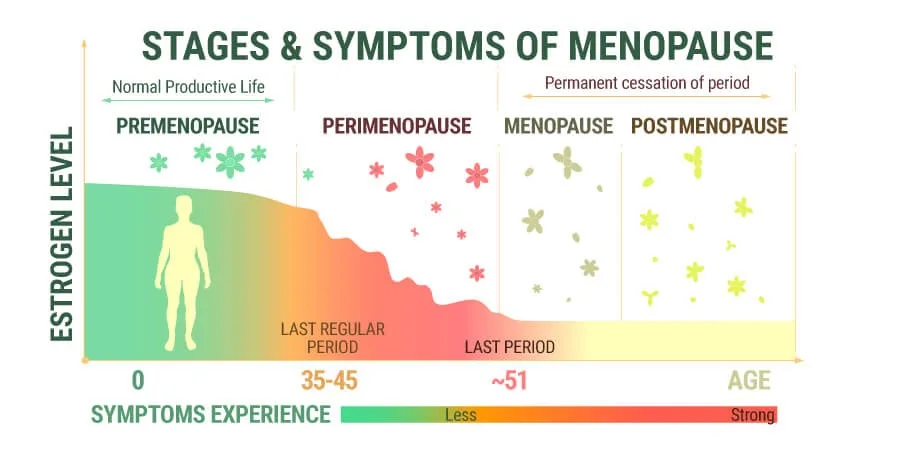
Numerous menstruation illnesses are largely caused by hormonal imbalances. The regular menstrual cycle can be thrown off by fluctuations in the amounts of hormones such as luteinizing hormone, progesterone, and estrogen. Hormonal imbalances, irregular or nonexistent periods, and diseases including polycystic ovarian syndrome (PCOS) and hypothalamus dysfunction can all be caused by these conditions.
Structural Abnormalities
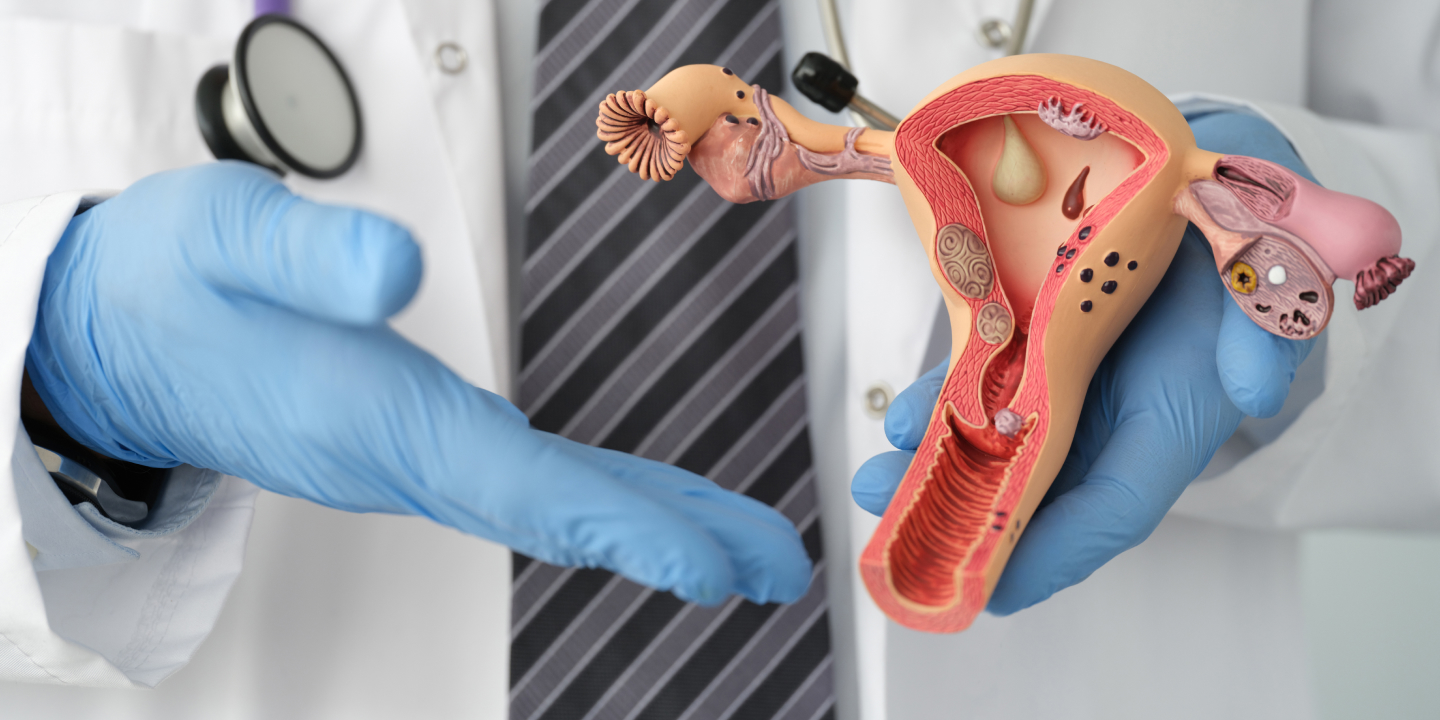
Menstrual problems can be brought on by structural abnormalities in the reproductive organs. Examples comprise:
- Uterine fibroids: These benign uterine growths can lead to significant or protracted bleeding.
- Polyps: Tiny, benign growths on the uterine lining may cause erratic bleeding.
- Adenomyosis: This condition occurs when the tissue lining the uterus invades the muscular wall, resulting in painful and protracted periods.
- Uterine Septum: A septum, or band of tissue, dividing the uterus partially or entirely, is a congenital abnormality that can affect fertility and cause irregular bleeding.
Thyroid Disorders
The thyroid gland produces metabolism-regulating hormones. Both an underactive thyroid and an overactive thyroid can affect the menstrual cycle, resulting in irregular or skipped periods.
Gynecological Disorders
Some gynecological disorders might make menstruation disorders worse. These consist of:
- Endometriosis: Endometriosis is a disorder in which the uterine lining tissue spreads outside the uterus, causing excruciating pain, copious bleeding, and irregular menstrual cycles.
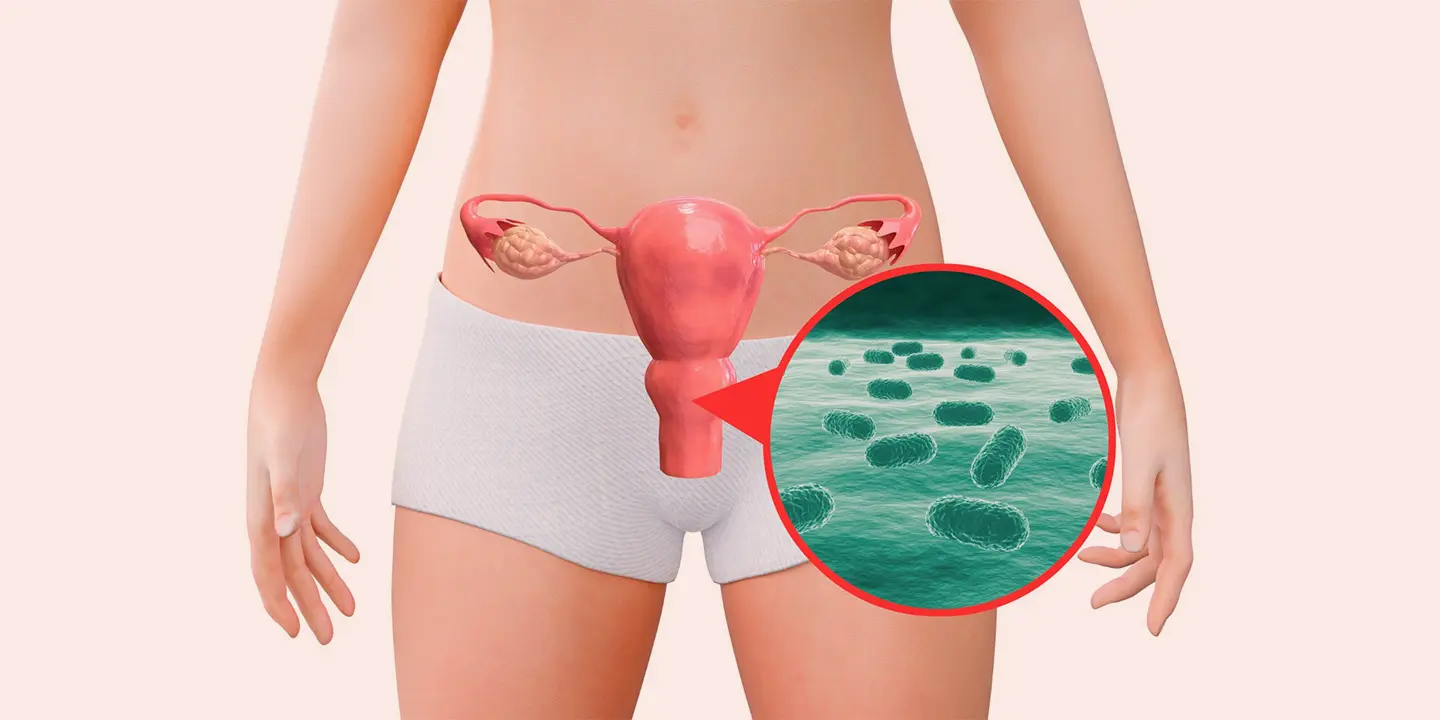
- Pelvic Inflammatory Disease (PID): SSTIs frequently contribute to PID, an infection of the reproductive organs. Pelvic discomfort and erratic bleeding are possible effects.
- Ovarian cysts: These fluid-filled sacs on the ovaries have the power to alter the menstrual cycle and proper hormonal equilibrium.
Medications and Contraceptives
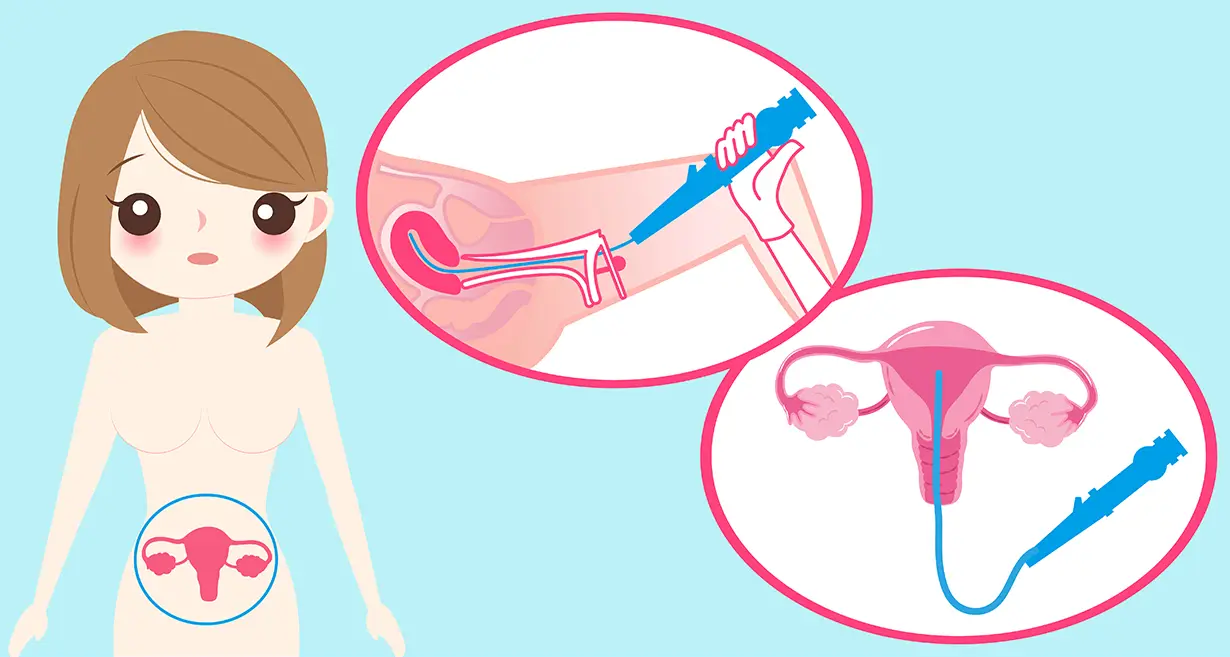
A number of drugs, including several antidepressants and anticoagulants, might alter menstrual bleeding patterns. The menstrual cycle may also be impacted by some types of contraception, including hormonal birth control methods and intrauterine devices (IUDs).
Lifestyle variables
A number of lifestyle variables, such as the following, might cause menstruation disorders:
- Excessive Exercise: Strenuous exercise or intense physical activity can upset the body’s hormonal balance and cause irregular or nonexistent periods.
- Chronic stress: Chronic stress has the potential to alter hormone levels and disrupt the regular menstrual cycle.
- Significant Weight Fluctuations: Rapid weight gain or reduction might mess with your hormones and make your periods irregular.
Diagnosis of Menstrual Disorders
An extensive examination by a healthcare professional is necessary for the diagnosis of menstruation disorders in order to pinpoint the underlying cause and choose the best course of action. The main steps in the diagnosis of menstruation problems are as follows:
Review of medical history
The medical professional will start by learning about your menstrual cycle, including the frequency, length, and other details of your periods. They will also ask about any relevant medical history, medications, and lifestyle variables, as well as any related symptoms. This data aids in creating a foundational understanding of your menstrual health.
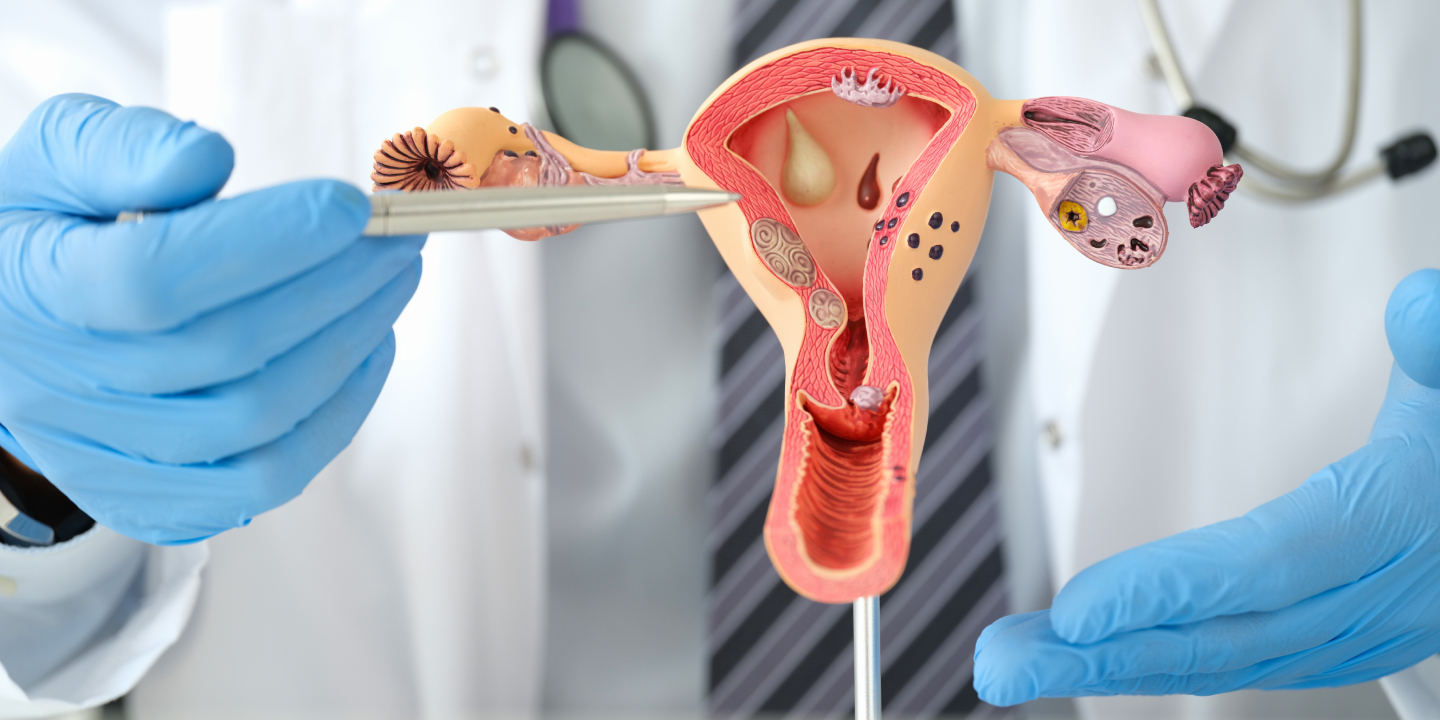
Physical Examination
To evaluate the condition of your reproductive organs, a physical examination may be performed. This may include a pelvic exam. The healthcare professional will check the uterus, ovaries, and cervix during the pelvic exam for any indications of abnormalities, such as cysts, fibroids, or infections. The physical examination may reveal important information about the possible origins of menstruation problems.
Blood Tests
Blood tests may be required to assess thyroid function, determine any underlying medical issues, and monitor hormone levels. Estrogen, progesterone, follicle-stimulating hormone (FSH), and luteinizing hormone (LH) levels can be used to analyze hormonal imbalances and identify the cause of irregular or nonexistent periods.
Imaging Studies
To view the reproductive organs and look for any anatomical irregularities, imaging studies may in some situations be advised. Ultrasound is a widely used imaging method that can be used to detect diseases such as ovarian cysts, polyps, and uterine fibroids. Magnetic resonance imaging (MRI) or computed tomography (CT) scans may be used in more complicated situations.
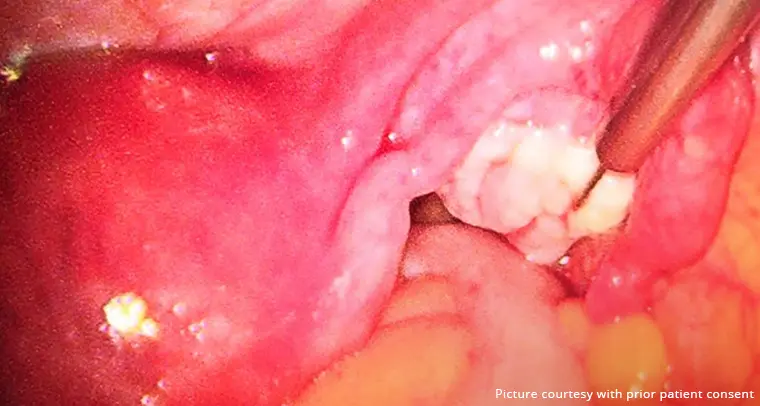
Biopsy
Endometrial biopsy may be advised if the medical professional detects abnormalities in the uterine lining (endometrium). A tiny sample of the uterine lining is removed during this operation for laboratory testing. It aids in excluding diseases like cancer or endometrial hyperplasia.
Monitoring Menstrual Patterns
Monitoring your menstrual cycles and accompanying symptoms using a period diary or smartphone app can help with diagnosis. In order to aid in the diagnostic process, this record can be used to spot any trends or inconsistencies in your menstrual cycle.
Treatment Of Menstrual Disorders
The precise ailment and its underlying cause will determine the menstrual disorder’s specific treatment. The main objectives of therapy are to control symptoms, control menstrual periods, and enhance a woman’s general quality of life. The following are some typical menstrual problems treatments:
Hormonal Therapy
To control the menstrual cycle and maintain hormone balance, hormonal therapy is frequently administered. To maintain a constant hormonal balance, may entail using birth control pills, patches, or hormonal intrauterine devices (IUDs). Hormonal therapy can help treat symptoms like painful menstruation, excessive bleeding, and irregular periods.
Nonsteroidal Anti-Inflammatory Drugs (NSAIDs)
NSAIDs, such as ibuprofen or naproxen, are frequently used to treat dysmenorrhea (menstrual cramps) and lessen excessive bleeding. These drugs function by lowering inflammation and preventing the synthesis of prostaglandins, which are responsible for painful uterine contractions.
Surgical Interventions
In some circumstances, it may be required to have surgery to correct underlying structural issues or other diseases that are related to menstruation disorders. Surgical techniques include, for instance:
- Hysteroscopy: A narrow, illuminated device (a hysteroscope) is inserted through the cervix during hysteroscopy, a minimally invasive technique, to view and treat uterine abnormalities such as polyps or fibroids.
- Endometrial ablation: To lessen heavy monthly bleeding, this surgery involves removing or dissolving the uterine lining. Usually, women who no longer want to have children are advised to do so.
- Myomectomy: When uterine fibroids are present, the uterus may still be preserved after a myomectomy to remove the fibroids.
- Hysterectomy: A hysterectomy may be advised in extreme instances or when other therapeutic alternatives have failed. The uterus and, in certain situations, the cervix must be surgically removed in order to do this. It is a permanent cure for some illnesses, but it also makes it impossible to get pregnant again.
Changes in lifestyle
Some lifestyle adjustments can aid in the management of menstruation problems. These may consist of:
- Stress management: methods include breathing exercises, meditation, and regular exercise. These methods can help lower stress levels and balance hormones.
- Exercise on a Regular Basis: Physical activity on a regular basis can assist control hormone levels and enhance general wellbeing. Excessive exercise should be avoided, though, as it can mess with your period.
The precise diagnosis, the intensity of the symptoms, personal preferences, and future fertility objectives all influence the therapy option. To choose the best course of action for properly treating menstruation issues, you must speak with a healthcare expert. It is normally advised to schedule frequent follow-up appointments to assess development and make any required modifications to the therapeutic strategy.
Takeaway
The quality of life and general health of a woman can be greatly impacted by menstrual diseases. Keep in mind that maintaining good menstruation health is crucial to overall wellness. If you are experiencing any menstrual irregularities or distressing symptoms, it’s important to consult specialists at Queen’s Gynecology for a proper diagnosis and appropriate treatment. Because of its skilled medical staff, extensive diagnostic tools, individualized treatment programs, and dedication to patient care, Queen’s Gynaecology is your safest choice for treating menstruation issues. For the best results, they use a multidisciplinary approach to address each individual’s needs and deliver high-quality, compassionate care.
Frequently Asked Questions
Normal menstruation is defined as having a cycle that lasts between 21 and 35 days with bleeding that lasts between 2 and 7 days. However, if you have any worries or see any noticeable changes in your menstrual cycle, you should speak with a healthcare professional to better understand your symptoms.
Yes, with the right care, the majority of menstruation disorders can be properly treated. The type of disease and its underlying cause will determine the therapy strategy.
Yes, hormonal birth control techniques like pills, patches, or IUDs can help manage heavy bleeding, normalize menstrual periods, and reduce pain.
If you have excruciating pain, continuous bleeding that interferes with your everyday activities, or any other substantial changes in your menstrual cycle, it is best to visit a doctor.