In this Article
What is the human papillomavirus infection?
Human papillomavirus HPV infection is a type of viral infection that spreads via skin-to-skin contact from person to person. There are more than 100 different types of HPV, more than 40 of which are sexually transmitted and can harm your mouth, throat, and genitalia.
HPV is the most prevalent sexually transmitted illness (STI), according to the Centers for Disease Control and Prevention (CDC).
It will happen to the majority of sexually active persons even if they have few sexual partners, at some point since it is so widespread and prevalent.
There may be cases of genital human papillomavirus infection that have no apparent negative health consequences. However, some kinds of HPV can result in the growth of genital warts as well as throat, cervix, and anus cancers.
HPV causes
Now that you have learned what is HPV, let us read about what are the possible HPV causes.
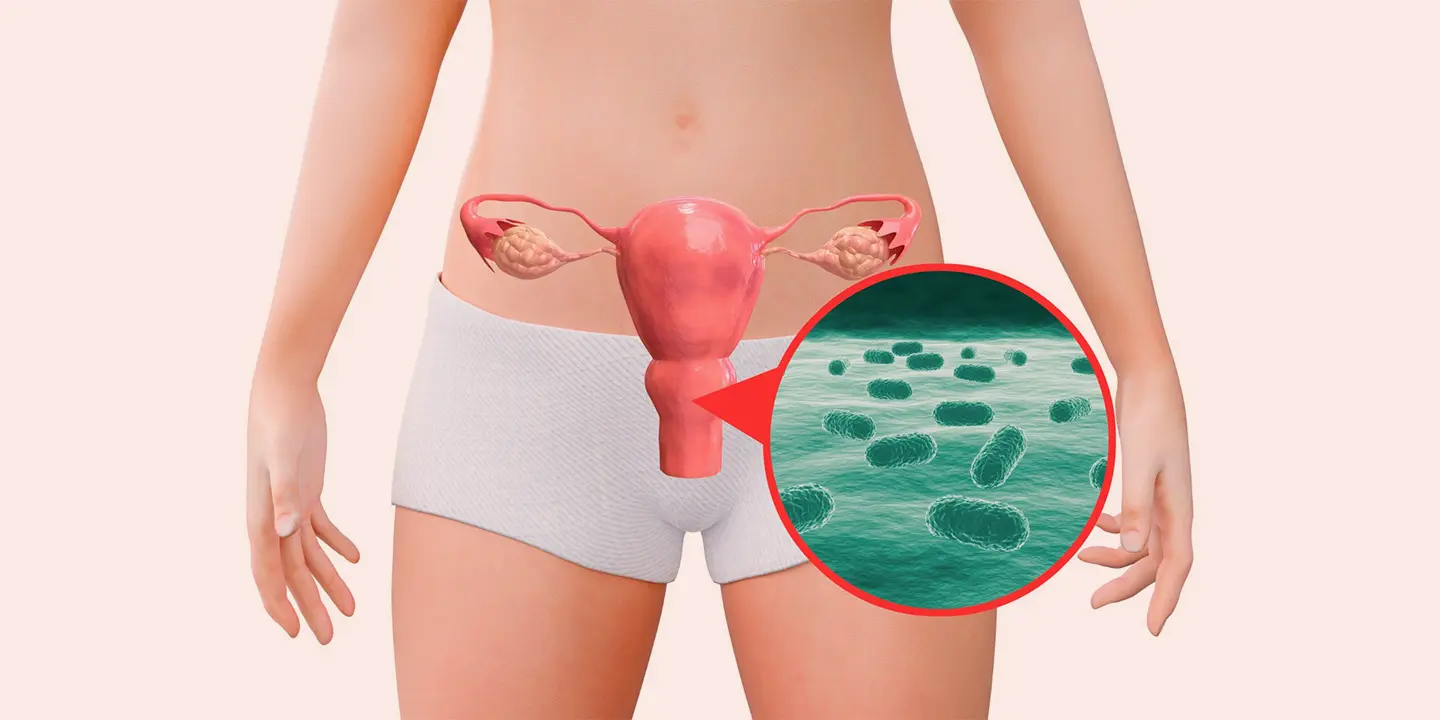
The main method of transmission for the virus caused by the HPV infection is skin-to-skin contact. Mostly the genital human papillomavirus infection is acquired through intimate physical contact, such as vaginal, anal, and oral sex.
Since it is a skin-to-skin virus, sexual activity is not necessary for the transmission of HPV to take place. Even if your partner shows no symptoms, you can still catch human papillomavirus HPV because many people carry the disease without even being aware of it. Additional HPV subtypes are also possible.
Rarely, an HPV-positive mother may pass the virus to her unborn child while giving birth. When this occurs, the kid may experience recurrent respiratory papillomatosis, a condition in which warts associated with HPV appear in the throat or airways.
HPV symptoms
There are no symptoms or health issues associated with HPV infection.
According to the CDC, 9 out of 10 HPV infections resolve on their own in less than two years. However, they could unintentionally spread the HPV virus because it may still be present in a person’s body at this time.
When a human papillomavirus infection becomes persistent, the effects on one’s health can be detrimental, causing the person to develop HPV symptoms such as throat warts and genital warts (known as recurrent respiratory papillomatosis).
Additionally, cancers of the genitals, head, neck, and throat as well as cervical cancer can be attributed to human papillomavirus infection (HPV).
The HPV strains which typically cause a person to develop warts are distinct from those HPV strains that result in cancer. Thus, having genital warts due to HPV does not make you predisposed to cancer.
Symptoms of HPV-related cancers frequently don’t appear until the disease has progressed to a more advanced stage. Regular exams can aid in detecting HPV-related health issues early. This can improve outlook and raise survival chances.
Men and HPV
The majority of males who get infected with HPV don’t show any symptoms, while some may have genital warts. If you find any strange lumps or lesions on your penis, scrotum, or anus, consult a physician.
Men who have certain HPV strains may develop throat, anal, and penile cancer. Males who engage in anal intercourse and those with compromised immune systems may be more susceptible to HPV-related cancers than other men.
The HPV strains that result in genital warts and cancer are distinct from one another.
HPV in women
According to estimates, at least one kind of HPV will be contracted throughout a woman’s lifetime by 80% of all females. Similar to men, many women who have HPV don’t exhibit any symptoms, and the infection resolves without endangering their health.
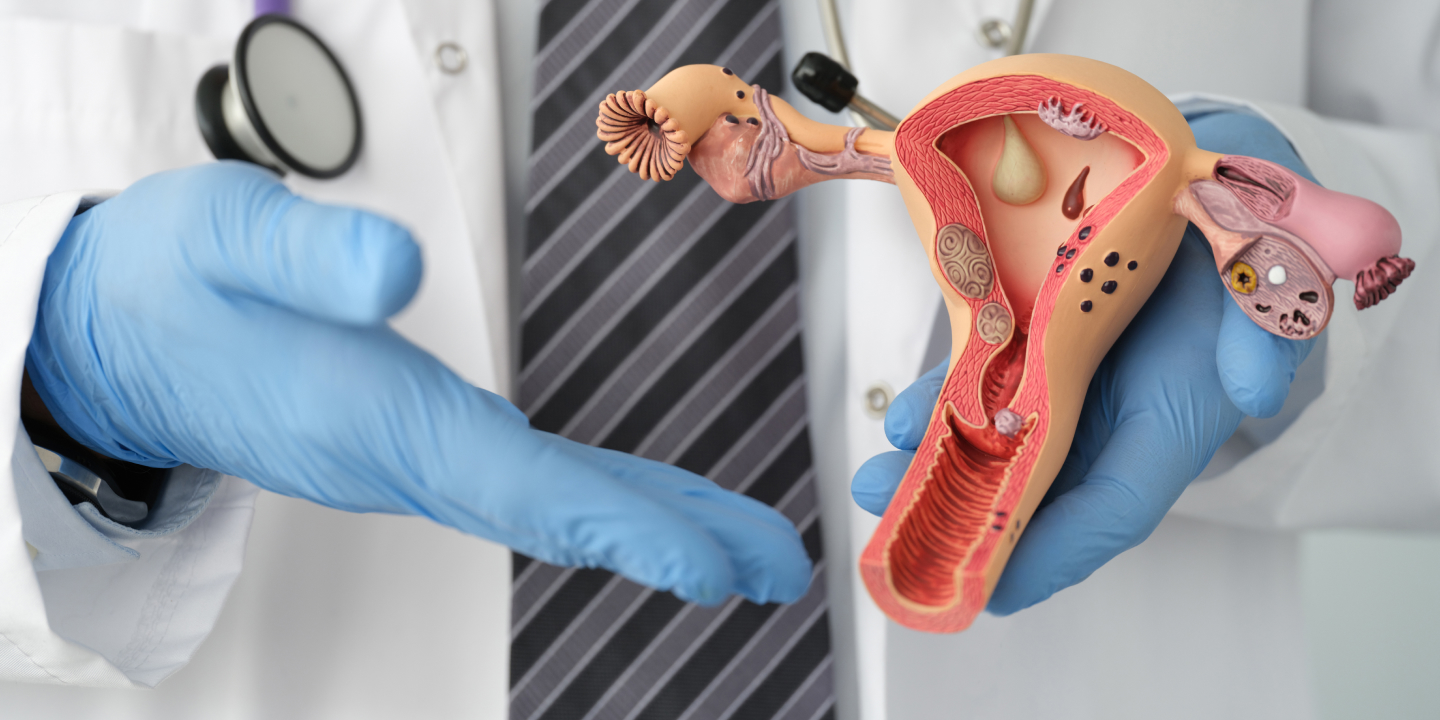
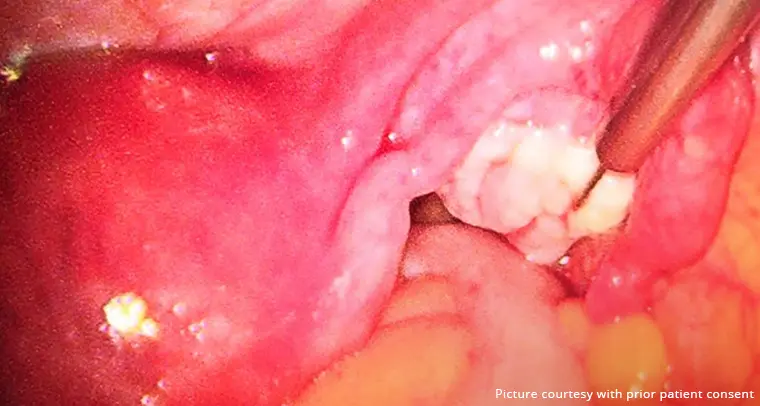
Genital warts, which can occur inside the vagina, in or around the anus, and on the cervix or vulva, may be discovered by some women.
If you discover any inexplicable lumps or growths in or near your genital region, schedule a visit with your doctor.
Certain HPV strains have been linked to throat, vaginal, or anus cancers as well as cervical cancer. The changes linked to female cervical cancer can be found with regular screening.
Furthermore, strains of HPV associated with genital cancers can be detected by cervical cells’ DNA tests.
Getting regular Paps smear tests for screening cervical cancer is significant. But it’s crucial to know that just because someone has a strain of HPV or cervical dysplasia doesn’t necessarily mean that they’ll get cancer.
How does HPV affect cervical cancer risk?
Most frequently, types 16 and 18 specific strains of HPV cause alterations to the cells of your cervix which results in a disorder known as Cervical dysplasia. The cervix is the gap between your vagina and uterus in females. If left untreated, a complication like Cervical dysplasia can progress to cervical cancer.
Most HPV infections go away on their own if you’re under 30. The frequency of testing should be decided at the age of 30 if HPV is discovered during a Pap smear (a test that checks for cervical cancer). You can be at a higher risk and require more frequent testing if you test positive.
How does HPV spread?
Skin-to-skin contact during sexual activity, oral sex, and anal sex are the three main ways that genital HPV spreads, making it extremely contagious. If the same body parts on an infected partner come into contact with your genitals, which include your vulva, vagina, cervix, penis, and scrotum, as well as your rectum and anus, you could become infected. The virus can be transmitted without exchanging any bodily fluids, and by hand-to-genital contact, as well. Even if no one ejaculates, you can still infect your partner or they can infect you.
Other elements that could enhance a person’s risk of contracting HPV include:
- more sexual partners overall
- unprotected oral, vaginal, or anal sex
- a compromised immune system
- having an HPV-positive sexual partner
The following can increase the possibility that a high-risk HPV-type infection may persist, possibly leading to cancer:
- a compromised immune system
- additional STIs such herpes simplex, gonorrhoea, and chlamydia
- persistent inflammation
- having a large number of children(cervical cancer)
- using oral contraceptives continuously for a long time (cervical cancer)
- the use of tobacco products (mouth or throat cancer)
- engaging in anal sex (anal cancer)
HPV tests
Testing for HPV differs for men and women.
Women
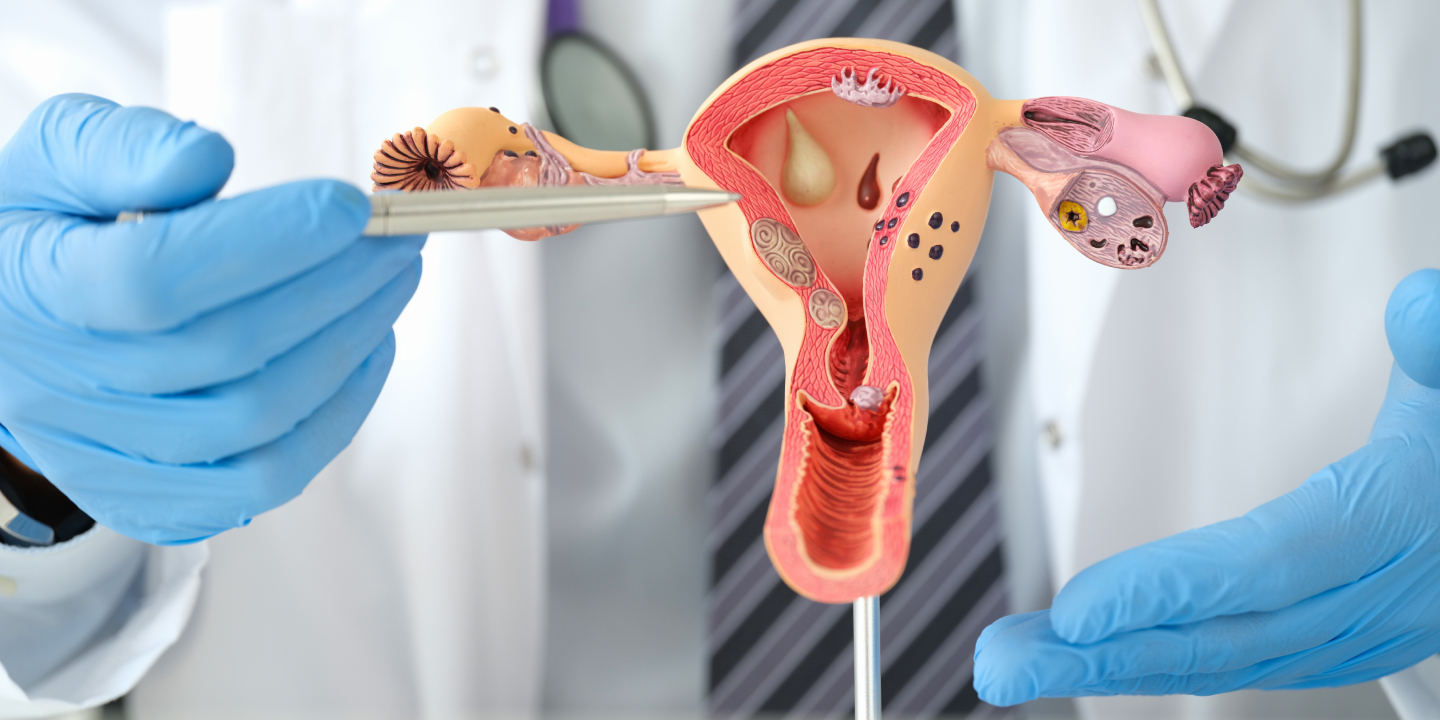
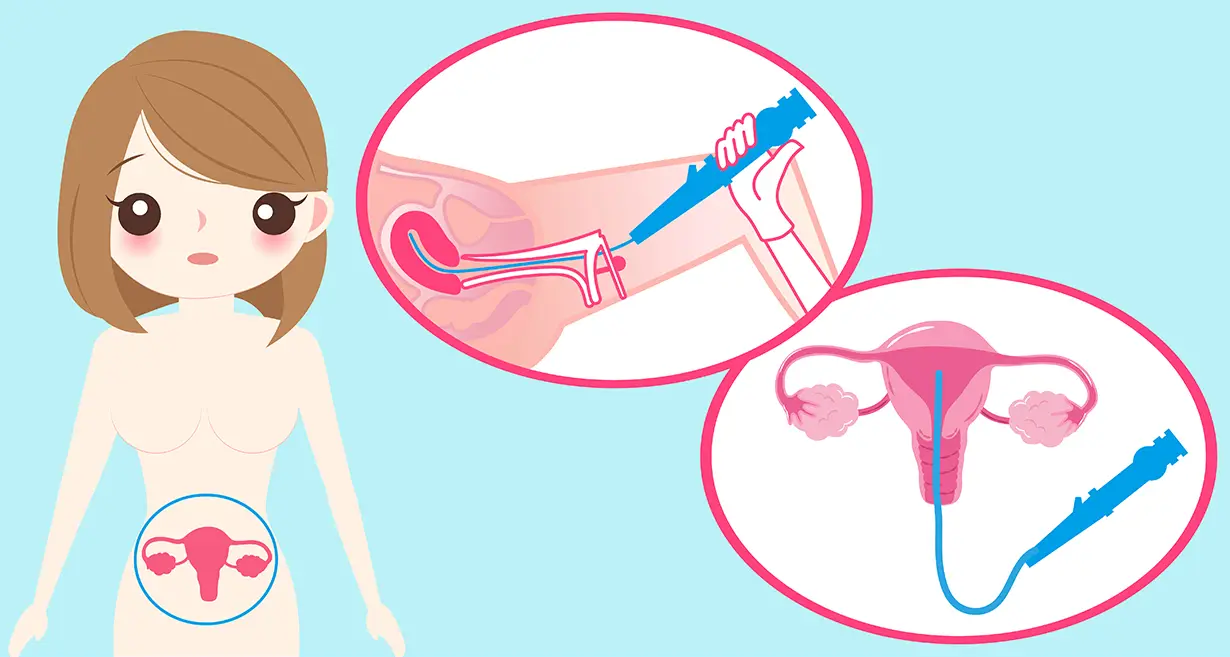
Regardless of when they first engage in sexual activity, women should get their first Pap test, also known as a Pap smear, at age 21, according to revised recommendations from the US Preventive Services Task Force (USPSTF).
Women with abnormal cells can be identified with regular Pap testing. These may indicate HPV-related issues or cervical cancer.
Just a Pap test every three years is recommended for women between the ages of 21 and 29. Women between the ages of 30 and 65 should choose one of the following:
- Every three years have a Pap test.
- Every five years, get screened for high-risk HPV types with an HPV test (hrHPV)
- Every five years, receive both assessments collectively; this is referred to as co-testing.
According to the USPSTF, standalone tests are favored over co-testing.
If the results of your Pap test are abnormal and you are under the age of 30, your doctor or gynecologist may additionally recommend an HPV test.
You could require more frequent Pap tests. A colposcopy, for example, may be recommended as a follow-up procedure by your doctor.
Infections with HPV frequently fade away on their own without generating cancer, and cervical alterations that eventually result in cancer frequently take several years to manifest. Instead of receiving treatment for abnormal or precancerous cells, you could wish to adopt a careful waiting strategy.
Men
The HPV DNA test is only available to diagnose HPV in women, it’s vital to remember that. Men can’t currently be diagnosed with HPV using an FDA-approved test. The CDC states that men are not now advised to undergo routine screening for the anal, throat, or penile cancer. For males who have a higher chance of developing anal cancer, some doctors may do an anal Pap test. Males with HIV and men who receive anal sex are included in this.
HPV treatments
There is no cure for HPV because the majority of cases go away on their own. Instead, your physician will probably request that you undergo more testing in a year to determine whether the HPV infection has persisted and whether any cell alterations have arisen that require further investigation.
It is possible to treat genital warts using prescription drugs, electrical current burning, or liquid nitrogen freezing. However, eliminating the physical warts does not treat the virus, and the warts may come back.
A quick procedure that is done in your doctor’s office can eliminate precancerous cells. Treatment options for cancers caused by HPV include surgery, radiation therapy, and chemotherapy. Multiple techniques may occasionally be employed.
There are no HPV treatments with natural remedies that are currently approved by medicine.
For the purpose of diagnosing, monitoring, and treating health issues that may arise from HPV infection, routine screening for HPV and cervical cancer is crucial.
Prevention of HPV
The only way to avoid contracting HPV is to avoid having intercourse. For many, more practical objectives include lowering the risk of HPV infection and preventing cervical cancer while continuing to engage in safe sex and lead a healthy sex life.
You can lower your risk If you:
Obtain the HPV vaccination- Getting vaccinated against HPV before engaging in sexual activity is the greatest approach to protect yourself from it. For the prevention of genital warts and cancers brought on by HPV, there is the Gardasil 9 vaccine. It is appropriate for all ages, 9 to 45. You may be protected from HPV strains from vaccinations you haven’t been exposed to. Find out from your doctor whether they advise being vaccinated.
Boys and girls should get the HPV vaccine by age 11 or 12, according to the CDC. The vaccine is administered in two doses at least six months apart. Ages between 15 to 26 including both women and men can also receive the Gardasil 9 vaccine in three doses.
Additionally, anyone between the ages of 27 and 45 who have not received an HPV vaccination before is now qualified to receive the Gardasil 9 vaccine.
Regularly undergo testing and screening- Cervical cancer is avoided via early HPV and abnormal cell detection. At age 21, you should start having routine Pap smears. You might require another Pap every one to three years or more, depending on your test results. You might require routine HPV testing just, routine Pap smears only, or both between the ages of 30 and 65. If you’re above 65, you could or might not require further screening. Discuss the screening schedule that makes sense for you with your provider.
Safe Sex should be practiced- Less efficient at preventing HPV than STIs that transmit by semen or vaginal fluid are condoms and dental dams. However, using them properly each time you have sex can lower your risk of contracting HPV.
Keep your partner(s) safe- If you have HPV, let your partner know so they may get tested as well. If you are receiving treatment for genital warts or high-risk HPV strains, you may need to cease having intercourse. Discuss with your doctor the safety measures you need to take if you have an HPV infection.
HPV and pregnancy
Your chances of getting pregnant are unaffected by contracting HPV. If you have HPV and are pregnant, you might want to postpone treatment until after delivery. However, HPV infection might occasionally result in difficulties.
Pregnancy-related hormonal changes may cause genital warts to spread and, in some circumstances, bleed. Widespread genital warts could make a vaginal delivery challenging.
A C-section can be necessary if genital warts prevent the birth canal from opening.
Rarely, a woman with HPV can transmit it to her unborn child. Recurrent respiratory papillomatosis, a rare but deadly illness, could develop as a result. Children who have this illness develop growths in their airways that are associated with HPV.
You should maintain your usual screening for HPV and cervical cancer while you are pregnant since cervical alterations can still happen.
What is HPV’s high risk?
HPV can lead to cancer in some cases. They are “high risk” as a result of this.
The way that cells communicate with one another is altered when a high-risk form of HPV infects them. The cells also get more numerous as a result. These cells are typically recognized by the immune system, which then controls them.
These aberrant cells, however, have the potential to develop into precancerous cells if they continue to exist.
The inner surface of various organs is lined with thin, flat squamous cells that are infected with HPV. Squamous cell carcinomas are the term used to describe the majority of HPV-related malignancies.
Adenocarcinoma is the term for the cancer that the virus can also induce in the glandular cells of the cervix.
HPV subtypes
More than 200 different kinds of HPV exist. They are divided into oncogenic and non-oncogenic groups by doctors.
At least 14 different HPV varieties have the potential to develop a malignancy.
Non-oncogenic kinds typically have no negative effects on one’s health. Non-oncogenic HPV strains are sometimes referred to as “wart-causing HPV” by doctors.
Frequently Asked Questions
HPV affects who?
Anyone who has sex or close skin-to-skin genital contact with a partner who has HPV can contract the virus. Similar to sexual contact, oral sex, anal sex, and another close genital touch, anyone infected with the virus can pass it to their partner.
Can HPV be cured?
No. The HPV virus cannot be cured. Your immune system can still successfully cleanse you of the virus thanks to its incredible power. About 90% of HPV infections disappear within a year or two.
Conclusion
Prevention of HPV is crucial in the fight against cervical cancer. This is why everyone should adhere to the CDC’s advice about vaccination. Though we would advise that you don’t automatically assume that you will develop cancer if you recently learned that you have HPV. Not every HPV variant is created equal. Although the HPV that causes genital warts might be embarrassing, the virus itself is not harmful. Most HPV infections can be cured by your body. Your doctor can keep an eye on cell changes in your cervix in situations where your body is unable to combat the infection. Regularly obtaining Pap screenings and HPV tests as advised can stop HPV from developing into cancer.
Since regular screening is crucial to diagnose HPV and its associated conditions, it is perfectly normal and calls for no cause for alarm as long as you have a supportive medical professional and a good team of doctors by your side. And that is what you get when you visit Queen’s Gynecology, Delhi.
At Queen’s Gynecology, the team of doctors is not only best equipped in dispensing the correct treatment, but they also provide legendary care on the principles of ethics, the latest technology, and the humane touch.