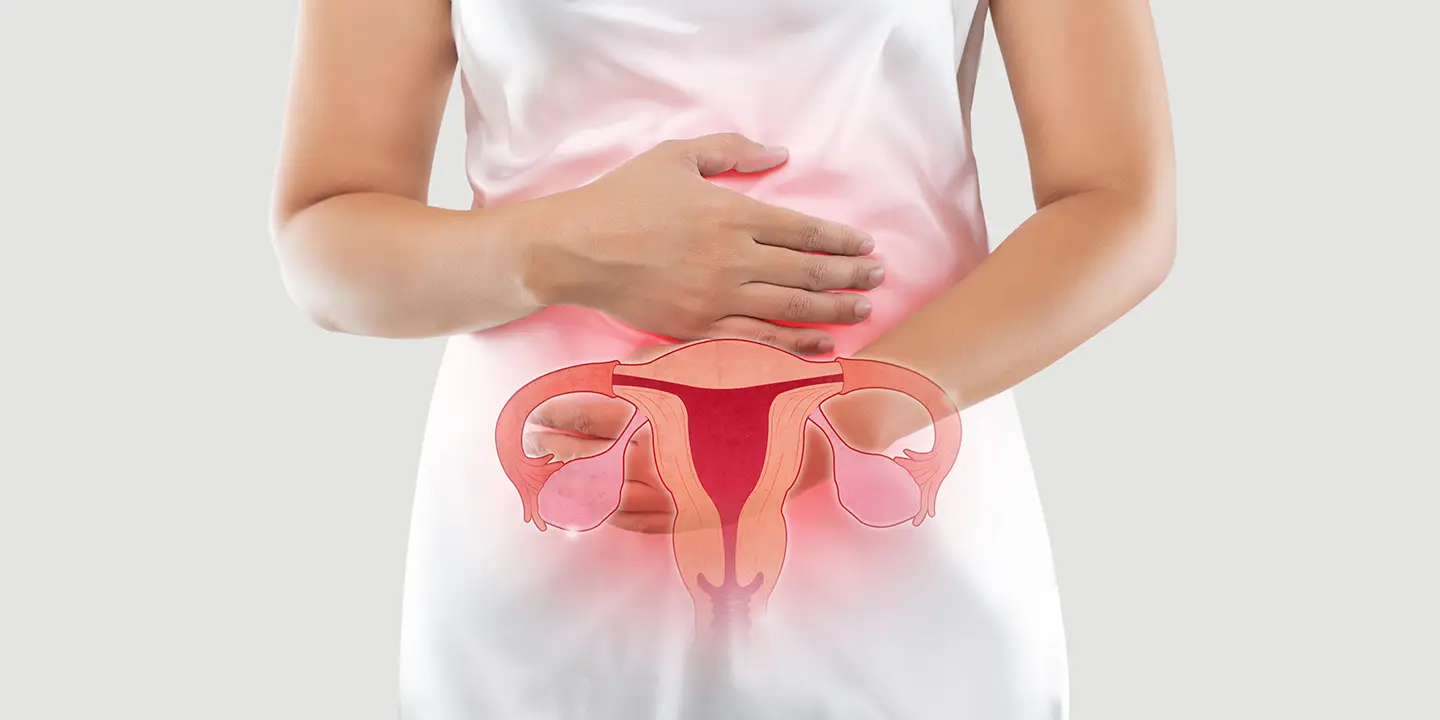
Millions of women throughout the world suffer from the persistent and even frequently painful ailment known as endometriosis. It happens when tissue resembling the uterine lining grows outside the uterus, causing inflammation, scarring, and a variety of other symptoms. The goal of this blog is to give readers a thorough understanding of endometriosis, including its causes, signs, symptoms, diagnosis, and available treatments. By bringing this disease to light, we hope to increase awareness, encourage early detection, and give women the confidence to get the care and assistance they need.
In this Article
- 1 Endometriosis
- 2 Causes And Risk Factors Of Endometriosis
- 3 Common Symptoms of Endometriosis
- 4 Diagnosis of Endometriosis
- 5 Treatment Options for Endometriosis
- 6 Fertility And Pregnancy Considerations
- 7 Effect Of Endometriosis On Fertility
- 8 Assisted Reproductive Technologies (ART)
- 9 Pregnancy and Management During Gestation
- 10 Takeaway
Endometriosis
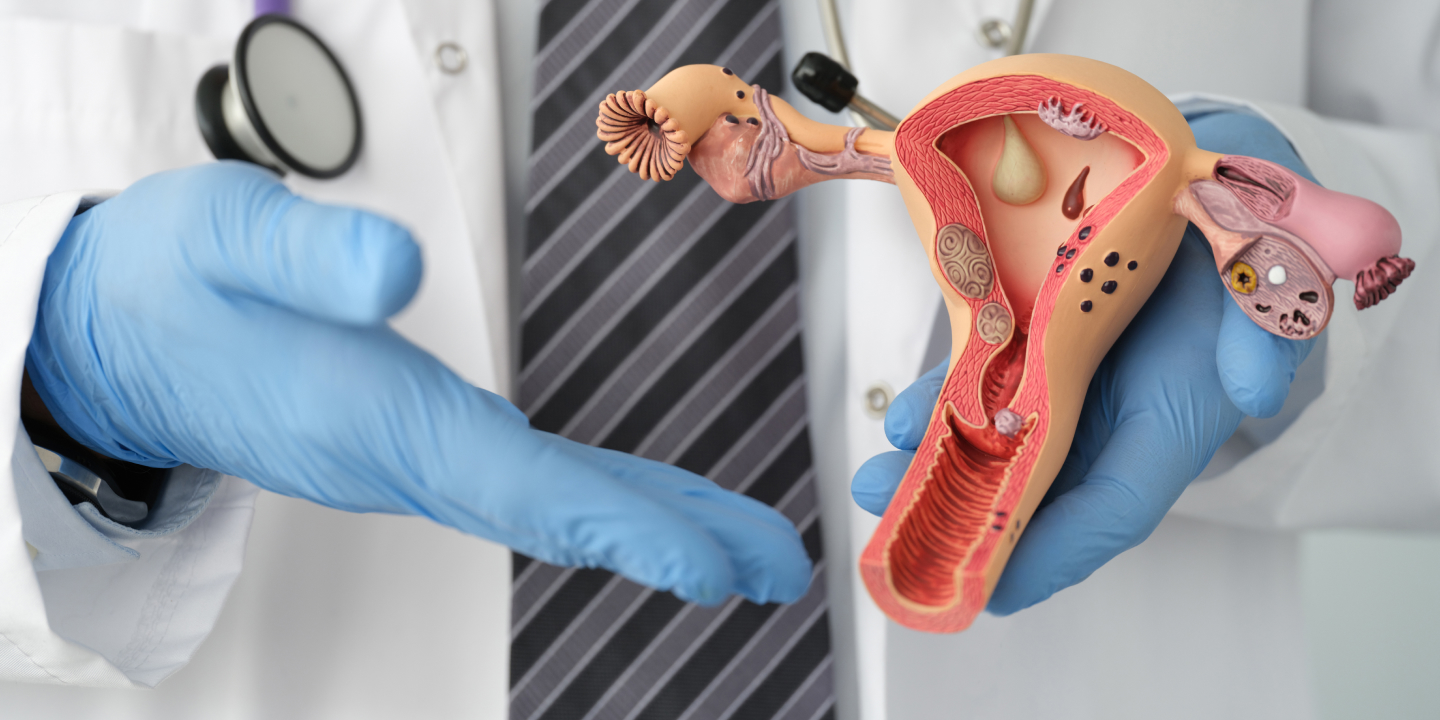
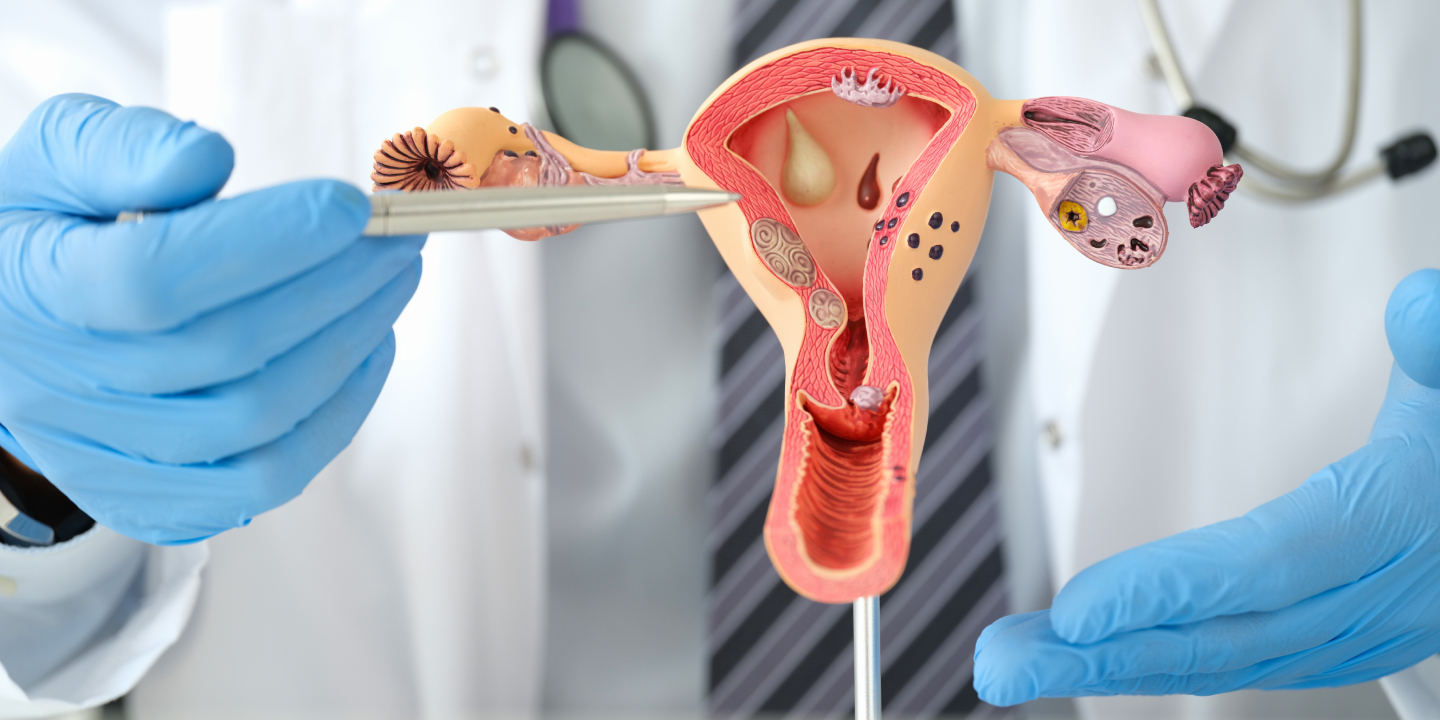
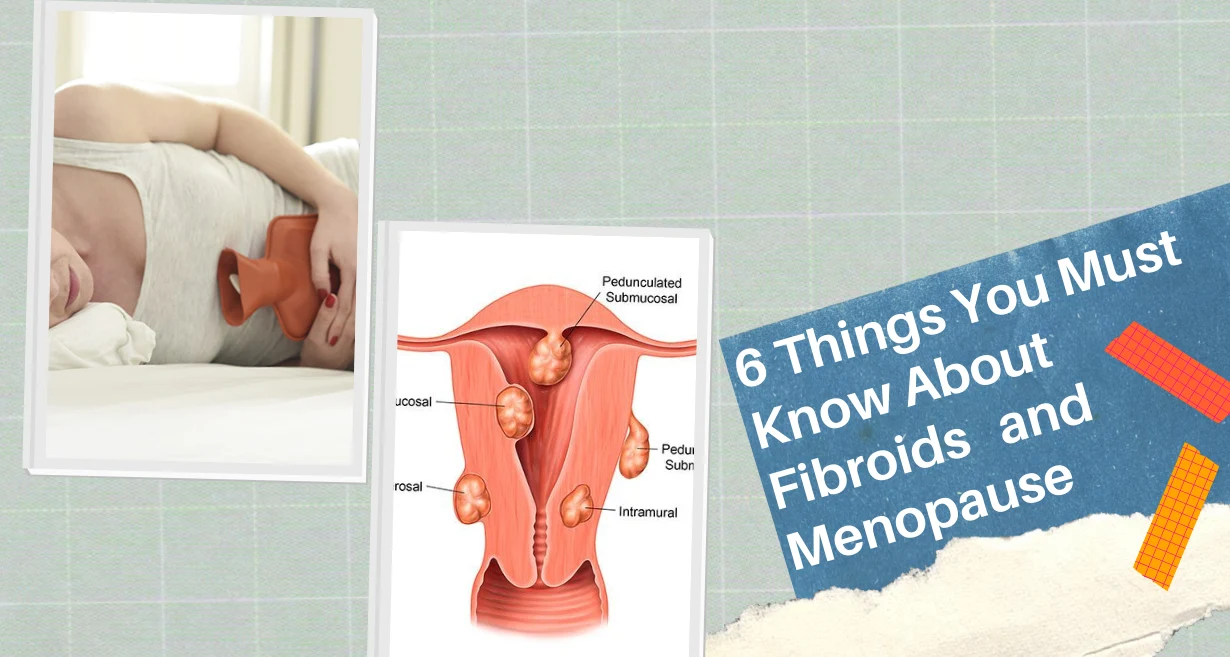
Millions of women throughout the world suffer from the chronic gynecological disorder known as endometriosis. It happens when the endometrium, or tissue that resembles the uterus’ lining, grows in organs like the ovaries, fallopian tubes, and the pelvic cavity. During the menstrual cycle, this displaced tissue reacts to hormonal fluctuations, which results in inflammation, scarring, and adhesion formation.
About 10% of women in the reproductive age group have endometriosis, making it a common disorder. It can significantly affect women’s health, resulting in symptoms like infertility, difficult periods, painful erections, and pelvic pain. Additionally, the illness may have emotional and psychological side effects that lower one’s quality of life and cause emotions of frustration and loneliness.
Endometriosis is a difficult and frequently misdiagnosed disorder. To control symptoms, protect fertility, and enhance general health, a good diagnosis, and a multidisciplinary strategy are necessary. In order to address the difficulties endometriosis-affected women confront and enhance their quality of life, greater knowledge, breakthroughs in research, and support are necessary.
Causes And Risk Factors Of Endometriosis
Although the precise etiology of endometriosis is still not entirely understood, many things are thought to play a role in its emergence.
Hormonal and Immune System Factors
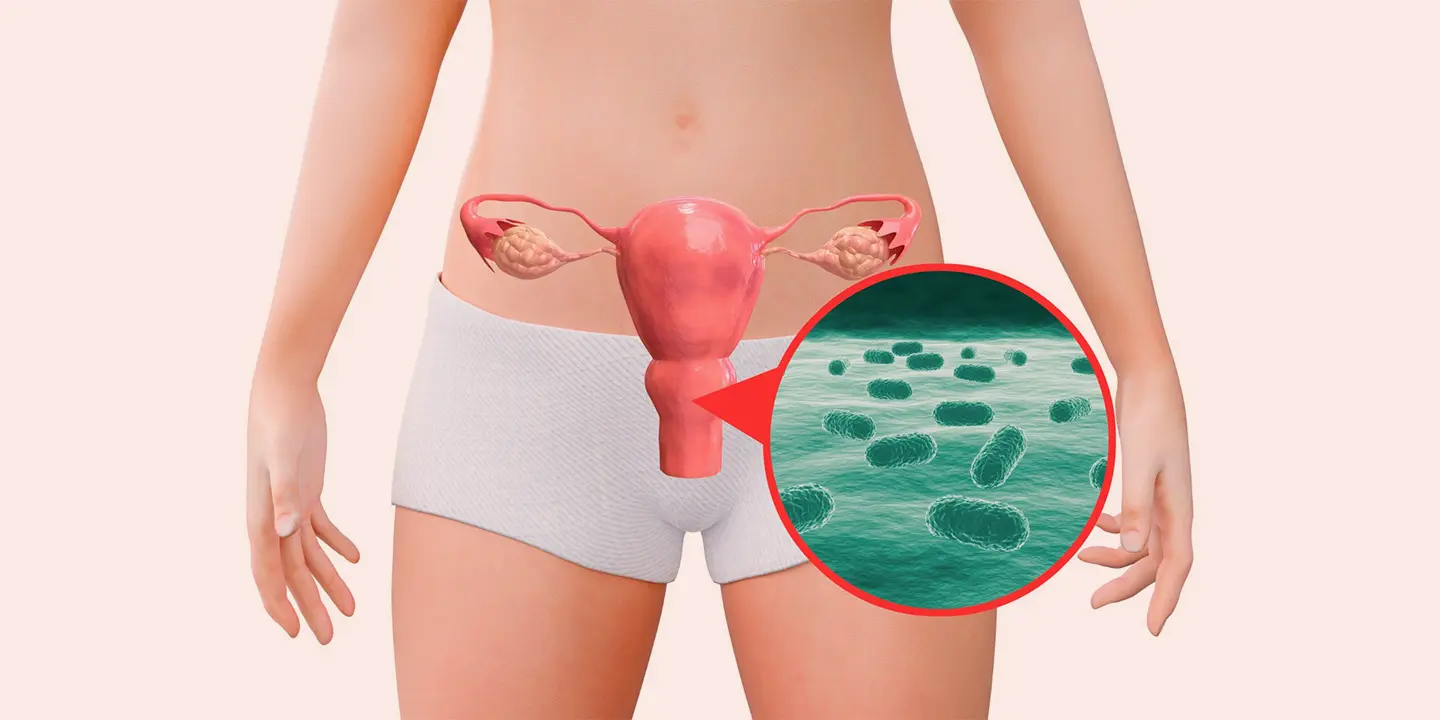
Endometriosis is often caused by hormonal abnormalities. Oestrogen can promote the unnatural growth of endometrial tissue outside the uterus. Oestrogen is the hormone that causes the uterine lining to thicken during the monthly cycle. Additionally, some immune system problems may make it difficult for the body to detect and get rid of displaced endometrial cells.
Genetic Predisposition and Family History
Endometriosis has a genetic component, and studies indicate that women who have close relatives (such as moms or sisters) who have the ailment are more likely to get it themselves. Endometriosis susceptibility may be increased by certain gene changes, however further study is required to identify the precise genes implicated.
Environmental and Lifestyle Factors
Endometriosis development may be influenced by environmental and lifestyle factors. Endometriosis risk has been associated with exposure to environmental pollutants such as dioxins and PCBs. These poisons can impair the immune system and hormone function. A higher incidence of endometriosis has also been linked to lifestyle variables such as excessive alcohol use, inactivity, and a high body mass index (BMI).
It’s crucial to remember that while these factors may raise the risk of endometriosis development, they do not ensure it. While some women with several risk factors may never develop endometriosis, many people with the disorder do not have any observable risk factors.
Related Blog – A Painful Tale of Endometriosis – Causes and Symptoms
Common Symptoms of Endometriosis
The symptoms of endometriosis can differ in severity from woman to woman and take many different forms. Some of the most typical signs of endometriosis include the following:
Pelvic discomfort and Cramping
One of the primary signs of endometriosis is pelvic discomfort. Chronic pelvic discomfort, which can be minor to severe, can affect women. The pain may be constant or sporadic and is frequently described as dull, aching, or intense, stabbing. Throughout the menstrual cycle, the pain’s severity can change, and it could get worse while you’re menstruating.
Painful Periods
Dysmenorrhea, or painful periods, is a common side effect of endometriosis for many female patients. The discomfort may radiate to the lower back and thighs and is often more severe than typical menstrual cramps. Daily activities may be hampered by the pain, which may need to be treated with medication.
Dyspareunia (discomfort during Intercourse)
Endometriosis can result in dyspareunia, or discomfort during sexual intercourse. The discomfort may be profound or superficial and may come on during or after sexual activity. It may cause sexual desire to decline and have an impact on the caliber of close relationships.
Heavy or Irregular Menstrual Bleeding
Menstrual bleeding that is heavy or irregular can be brought on by endometriosis. Women may suffer menstrual flow that necessitates routine pad or tampon replacements. Additionally, some women may experience irregular menstrual cycles, with their periods happening more frequently or less frequently than the typical 28-day cycle.
Gastrointestinal and Urinary Symptoms
Endometriosis can impact the gastrointestinal and urinary systems, causing symptoms like bloating, constipation, diarrhea, nausea, and pain when urinating or having bowel movements. Because of the close closeness of endometrial implants to these organs, these symptoms may be more noticeable during menstruation.
It’s crucial to remember that the degree of endometriosis does not always correspond with the intensity of the symptoms. While some females with moderate endometriosis may have substantial pain, others with more advanced illnesses may have little symptoms. Additionally, some women may not exhibit any symptoms at all, making a diagnosis difficult.
It is imperative to speak with a healthcare physician if you encounter any of these symptoms, especially if they interfere with your everyday life. For women with endometriosis, early detection and effective management can help reduce symptoms and enhance overall quality of life.
Related Blog – What Is UTI Infection? Causes, Symptoms, and Treatment infection of Urinary Tract Infection in Female
Diagnosis of Endometriosis
Due to the variety of symptoms, diagnosing endometriosis can be difficult. The most common techniques for diagnosing endometriosis are as follows:
Assessment of the medical history and symptoms
A thorough medical history discussion is required as the first step in the diagnosis of endometriosis. Your doctor will ask you about your symptoms, their frequency and intensity, and how they affect your day-to-day activities. Your menstrual cycle, pain patterns, and any conditions that make your symptoms worse or better can all be helpful in the diagnosing procedure.
Physical examination
A pelvic examination is frequently carried out to check for any palpable anomalies or endometriosis symptoms. Your doctor will feel the pelvic area for any sore spots, odd lumps, or nodules during the examination. It’s crucial to remember that not all cases of endometriosis may be found by a simple physical examination.
Imaging Techniques
Imaging tests like magnetic resonance imaging (MRI) and ultrasound can be used to visualize the pelvic organs and find any unusual growths or cysts that could be signs of endometriosis. Although these imaging methods can reveal useful information, they are not conclusive endometriosis diagnostic tools.
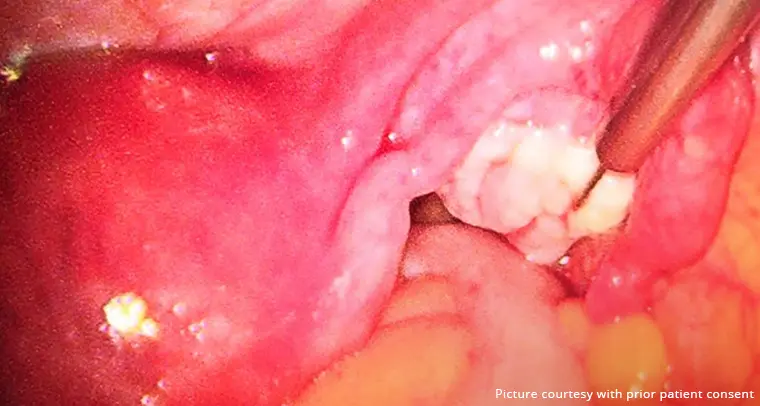
Laparoscopy and Tissue Biopsy
Undergoing a laparoscopy, a surgical procedure, under general anesthesia, is the most reliable way to diagnose endometriosis. A small abdominal incision is used to introduce a laparoscope, a thin, illuminated tool, during a laparoscopy. This enables the medical professional to see the pelvic organs and spot any endometrial adhesions or implants. A tissue biopsy may be performed if any suspicious lesions are discovered for additional investigation.
Being an intrusive procedure, laparoscopy should only be used in situations where there is a strong suspicion of endometriosis or when surgical intervention is required for therapy. It is crucial to speak with a healthcare specialist if your symptoms make you think you could have endometriosis. To find the best diagnostic strategy for your unique case, they will perform a complete evaluation.
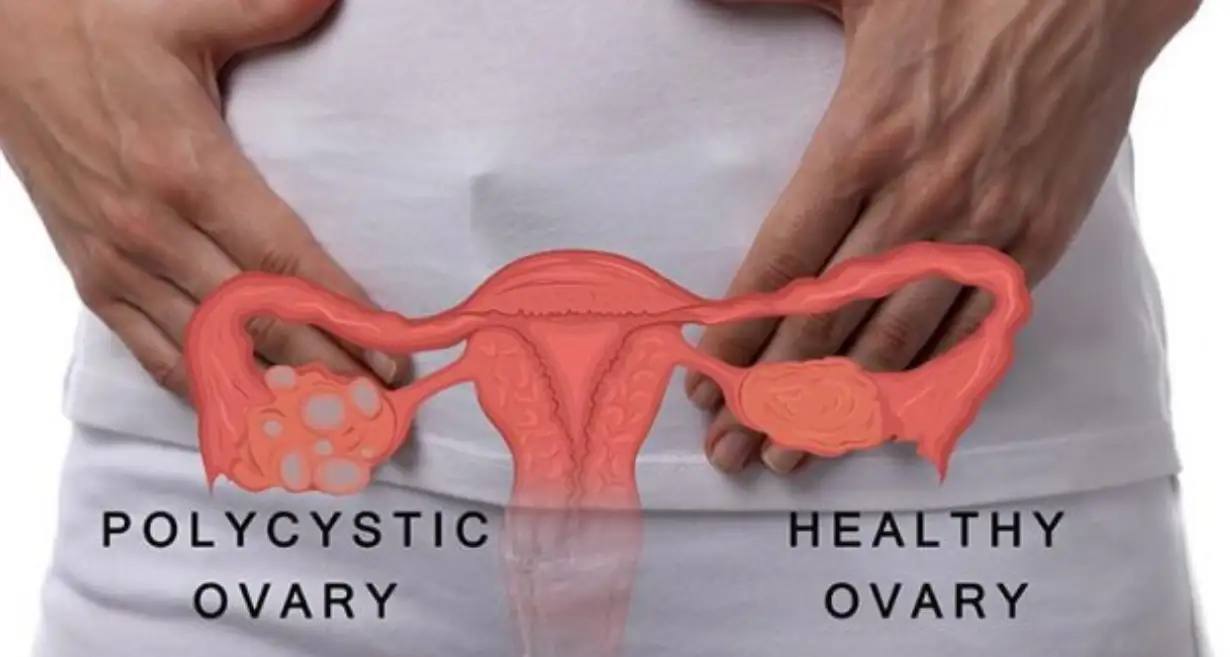
Related Blog – Polycystic Ovary Syndrome – Symptoms, Causes, as well as Treatment
Treatment Options for Endometriosis
Endometriosis management seeks to reduce symptoms, enhance quality of life, and protect fertility. The severity of the disease’s symptoms, the woman’s age, and her desire to become pregnant in the future all play a role in the treatment decision. The following are typical endometriosis treatment options:
Pain relief and symptom management
Nonsteroidal anti-inflammatory medicines (NSAIDs), which reduce inflammation and discomfort, may be prescribed to treat endometriosis-related pelvic pain and cramps. A heating pad or other form of heat therapy may also be helpful. In addition to medication therapies, lifestyle changes such as regular exercise, stress management methods, and dietary adjustments can help manage symptoms.
Hormonal therapy
Hormonal therapy seeks to inhibit estrogen production and lessen endometrial tissue growth and activity. Typical hormonal therapies include:
- Birth Control Pills: Oral contraceptives that include both progestin and estrogen can help control menstruation, lessen pain, and limit the formation of endometrial tissue.
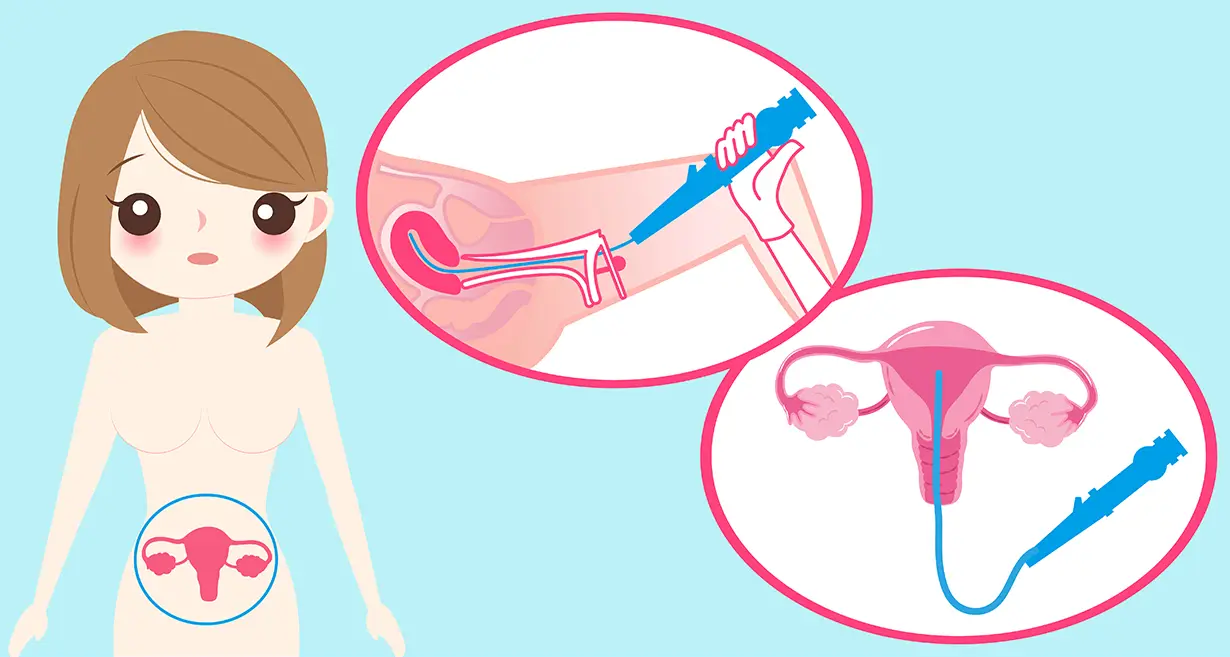
- Progestin Therapy: Progestin-only treatments, including pills, injections, and intrauterine devices (IUDs), can help treat symptoms and slow the development of endometrial tissue.
- GnRH Agonists: A condition resembling menopause is brought on by gonadotropin-releasing hormone (GnRH) agonists, which momentarily block estrogen production. Due to possible side effects, this is normally used as a short-term treatment to help shrink endometriosis lesions and lessen symptoms.
Surgical Interventions
When non-surgical treatments are ineffective or when a woman has moderate to severe endometriosis, surgery may be advised. There are two primary surgical methods for endometriosis:
- Laparoscopy: Endometrial adhesions, cysts, and implants can all be removed or destroyed by a minimally invasive treatment known as laparoscopy. It seeks to alleviate discomfort and return the pelvis to its ideal shape.
- Hysterectomy: When fertility is no longer an issue or when the condition is severe, a hysterectomy may be considered. The uterus, and occasionally the ovaries and fallopian tubes, are removed during this surgical surgery. Endometriosis can be permanently treated with a hysterectomy, but because of how it may affect fertility, this option should be carefully evaluated.
Endometriosis treatment is frequently tailored to the individual demands and objectives of each woman in order to best meet her needs. The effectiveness of the treatment must be monitored frequently so that the strategy can be changed as necessary.
It is important to remember that endometriosis is a chronic condition that may require long-term management, even though therapies can help manage symptoms and enhance the quality of life. After treatment, some women may experience symptom recurrence or may need continued treatment to keep symptoms under control.
Every woman’s experience with endometriosis is different, so it’s important to collaborate closely with medical professionals to determine the best course of action. Women with endometriosis can find relief, enhance their well-being, and carry on with their goals in life with the right management.
Related Blog – Menorrhagia (Heavy Periods)- Meaning, Symptoms, Causes And Treatment
Fertility And Pregnancy Considerations
A woman’s fertility may be significantly impacted by endometriosis, making conception more difficult. The development of adhesions, inflammation, and hormonal imbalances brought on by the presence of endometrial tissue outside the uterus might prevent regular reproductive functions. It’s crucial to remember, though, that not all women with endometriosis will have trouble getting pregnant.
Effect Of Endometriosis On Fertility
Endometriosis has a variety of effects on fertility. The reproductive organs may develop structural abnormalities as a result, such as clogged fallopian tubes, which may obstruct the path of the egg toward the sperm. Endometriosis can also interfere with or degrade the quality of an egg’s release from the ovaries. The inflammatory environment brought on by endometriosis can also interfere with an embryo’s capacity to implant in the uterus or the sperm’s ability to fertilize the egg.
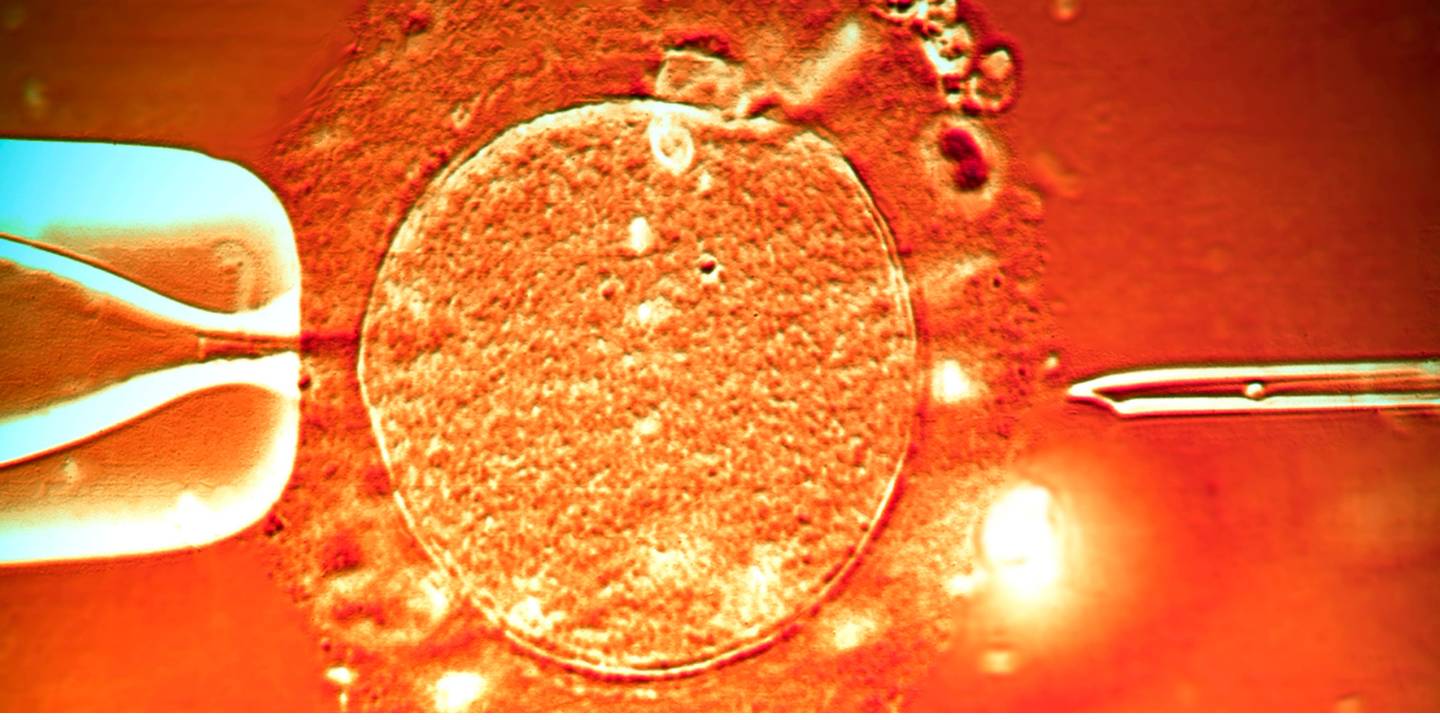
Assisted Reproductive Technologies (ART)
For endometriosis-affected women who are having trouble getting pregnant, ART may be suggested. These methods include in vitro fertilization (IVF), in which sperm and eggs are combined in a lab setting before being delivered to the uterus without first traveling through the afflicted fallopian tubes. In circumstances where conventional treatments have failed, ART can increase the likelihood of pregnancy in endometriosis patients.
Pregnancy and Management During Gestation
It’s crucial to carefully monitor a lady with endometriosis’s pregnancy and deal with any potential issues. While endometriosis by itself may not raise the risk of miscarriage, it may raise it for other pregnancy-related issues including preterm birth or cesarean delivery. Regular prenatal care, including careful pregnancy monitoring, can aid in identifying and managing any potential problems.
Some women may have a temporary improvement in endometriosis symptoms during pregnancy due to hormonal changes. It’s crucial to remember that symptoms could come back after childbirth or when hormone levels reach their pre-pregnancy levels.
Women with endometriosis should speak with a healthcare professional who specializes in reproductive health about their fertility issues and pregnancy plans. They can offer individualized advice and support, fertility treatments if required, and assistance in managing the disease while pregnant.
Takeaway
In addition to causing discomfort, fertility issues, and emotional suffering, endometriosis can have a considerable negative influence on a woman’s quality of life. Women can, however, get symptom alleviation and enhance their general well-being with early diagnosis and effective care.
When having endometriosis-related symptoms, it is imperative to consult a doctor and push for all-encompassing care. The best endometriosis therapy is available at Queen’s Gynaecology, which uses a multidisciplinary approach, skilled gynecologists, cutting-edge facilities, and individualized care.
Gynecologists, reproductive endocrinologists, and surgeons with endometriosis care experience form a multidisciplinary team at Queen’s Gynecology to help establish an accurate diagnosis and direct the best course of action. They put the needs of the individual first, offer extensive diagnostic and therapeutic alternatives, and work to enhance the well-being and quality of life of endometriosis-affected women.
Frequently Asked Questions
Endometriosis can indeed impact fertility but is not necessarily the direct cause of infertility. Inflammation, hormone dysregulation, and anatomical abnormalities that affect the reproductive system can result from it. However, not all endometriosis sufferers will have problems getting pregnant.
According to studies, endometriosis patients miss out on social gatherings, work, and education. Relationships with your partner, friends, children, and coworkers may be strained as a result of this health issue. In addition, endometriosis can make it challenging for a woman to conceive. When endometriosis interferes with fertility, surgical intervention can increase the likelihood of becoming pregnant.
There is currently no known cure for endometriosis. However, a number of treatments can aid in symptom management and enhance quality of life. The treatment plan is based on the needs and objectives of each patient.
After treatment, endometriosis may return, especially if the underlying immunological and hormonal variables are still present. It’s crucial to follow up with medical professionals on a regular basis to monitor symptoms and modify the course of treatment as necessary.
Speak with your doctor or obstetrician/gynecologist (OB/GYN) if you experience disease symptoms. Endometriosis can occasionally be confused with other medical conditions that can cause pelvic pain, and the precise cause may be difficult to determine.
No. No human being may contract endometriosis from another as it does not transfer. Endometriosis is not an infectious condition, however, its cause is not yet known.