Roughly 3 in every 4 women experience genital fungal infection, more commonly known as vaginal yeast infection, at least once in their lifetime. This goes to show that the condition is fairly common among women and is often a recurrent complication that women experience across the globe.
Besides sexual intercourse and poor vaginal hygiene, which are often considered the most common triggers of the infection, there are studies that indicate a potential correlation between diabetes and genital fungal infection.
More on that and the risks of diabetes fungal infection will be discussed at length in this article.
In this Article
- 1 Why is Treatment for Genital Fungal Infection a Necessity in Women?
- 2 Understanding the Correlation between Diabetes and Yeast Infection in Women
- 3 What are the Signs and Symptoms of Genital Fungal Infection?
- 4 What are Some Factors that Augment the Risks of Yeast Infections Induced by Diabetes?
- 5 What is the Mode of Diagnosis of Diabetes-induced Genital Fungal Infection?
- 6 How is Genital Fungal Infection Treated?
- 7 Are There Any Home Remedies that Help Treat Vaginal Yeast Infections?
- 8 What are some Preventive Measures for Genital Fungal Infection?
- 9 Conclusion
Why is Treatment for Genital Fungal Infection a Necessity in Women?
The treatment for genital fungal infections or yeast infections in women is often a medical necessity. Not only do they help relieve the symptoms, but it also prevents the risks of certain complications.
If left untreated, genital fungal infections can lead to complications. For example, recurrent or untreated infections can result in chronic discomfort and disruption of daily activities.
In some cases, the infection can spread to other parts of the body, causing systemic infections that may require more aggressive treatment. Prompt treatment helps prevent these complications.
Proper and on-time treatment is what our expert gynecologists at Queen’s Gynecology prioritize. Not only do they impose complications, but these kinds of one-time or recurrent vaginal infections are also associated with poor quality of life and social relationships.
Furthermore, misdiagnosis surrounding such infections is common in women. There are instances where the symptoms of genital fungal infections can sometimes mimic other conditions, such as bacterial vaginosis or sexually transmitted infections (STIs). Getting proper and on-time treatment is hence crucial for complete recovery.
Related Blog – HB Electrophoresis Test in Pregnancy: Normal Level, Procedure, And Cost
Understanding the Correlation between Diabetes and Yeast Infection in Women
The correlation between fungal infection and diabetes is often discussed and has a scientific background to it. Significant research depicts that unregulated or extremely high blood glucose levels, which are common in diabetes patients, can increase the risks of developing vaginal yeast infections.
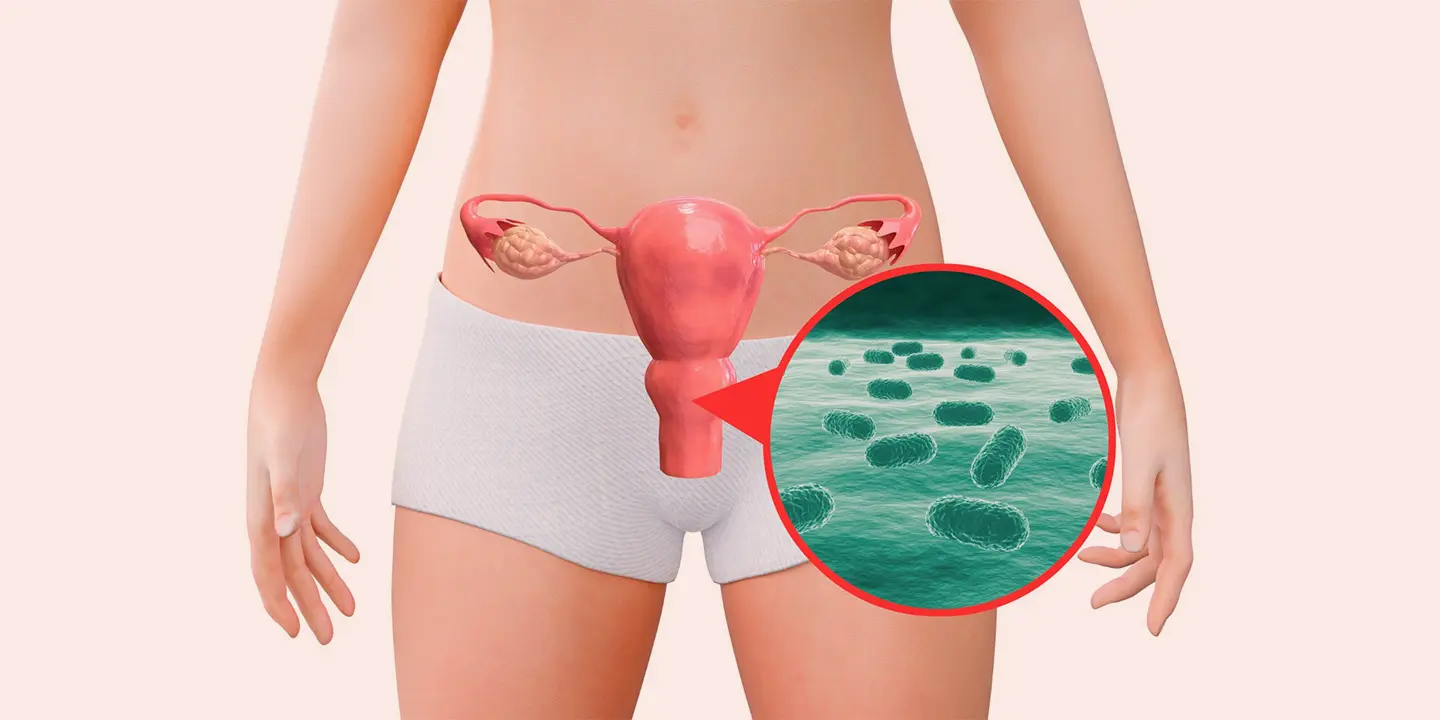
Yeast, which is the basis of fungal infections, is reliant on sugar for its propagation and proliferation in the body. Diabetes patients who generally have a high glucose level in their blood create an “ideal feeding ground” for the yeast to thrive and grow.
When the blood glucose levels aren’t regulated and are high, it helps the yeast to overgrow, thereby contributing to vaginal yeast infection in women. This is one of the primary reasons why diabetes patients are often advised to undergo regular screening for yeast infections and keep the risks at bay.
Even a 2018 study with over 300,000 subjects concluded that patients with diabetes (type 1 and type 2) often have a higher risk of developing a yeast infection compared to patients who don’t have diabetes.
Not just that, reports also depict that the “effectiveness” of the treatment of fungal infection due to diabetes is more difficult due to unregulated or high blood glucose levels. If not treated on time and eliminated, these infections can lead to profound complications.
What are the Signs and Symptoms of Genital Fungal Infection?
From the information shared until here, we have come to the conclusion that diabetes causes fungal infection. It is one of the potential contributing factors.
That said, identifying the symptoms of this type of fungal infection is essential. Following are a few of the symptoms of genital mycotic infections worth exploring:
- Intense itching
- Burning or pain during urination
- A slight odor from the genitals
- White or creamy discharge from the vagina
- Redness and swelling
- Pain while engaging in vaginal intercourse
- Itching on the exterior portion of the vagina
These are some of the most common symptoms. However, if you experience abdominal or back pain, yellow-colored discharge, and bleeding through the vagina, that warrants immediate medical intervention.
Related Blog – Menstrual Disorders — Types, Causes, Symptoms, Diagnosis, and Treatment
What are Some Factors that Augment the Risks of Yeast Infections Induced by Diabetes?
Unmanaged or unregulated diabetes often triggers the risks of yeast infections in patients. There are certain factors involved between yeast overgrowth and diabetes.
Following are a few factors worth exploring:
Compromised immune system
Studies indicate that uncontrolled diabetes often leads to a suppressed immune system. Research depicts that unmanaged blood glucose levels often suppress the functions of certain immune proteins called beta-defensins.
The lack of availability and proper functioning of these proteins leads to the overgrowth of the yeast in prone areas, leading to infection.
Extra sugar presence
The “yeast-friendly” areas in women include the genitals. Patients who have diabetes often pave the way for the yeast to attach itself to the skin cells and mucus glands, leading to an unhealthy level of growth and contributing to the infections that many women often struggle with.
Not just glucose, yeast infection also leads to the production and storage of glycogen, elevating the acidity in the vagina and thereby increasing the risks of infection in the genitals.
Recurrent or persistent infections
Another risk factor associated with diabetes genital fungal infection is recurring infections. If you aren’t getting proper treatment for diabetes and your sugar levels are through the roof or often unregulated, it might lead to the infection returning.
Determining and prioritizing these individual triggers is important, especially when it comes to the management of the condition.
What is the Mode of Diagnosis of Diabetes-induced Genital Fungal Infection?
Genital fungal infections often affect a woman’s quality of life. If you are experiencing any of the symptoms related to the vaginal infection, getting a timely diagnosis and treatment is crucial.
The diagnosis of the condition typically relies on the symptoms one is experiencing. Besides that, the basis of diagnosis also relies on the patient’s medical history, diabetes management treatment, blood glucose levels, etc.
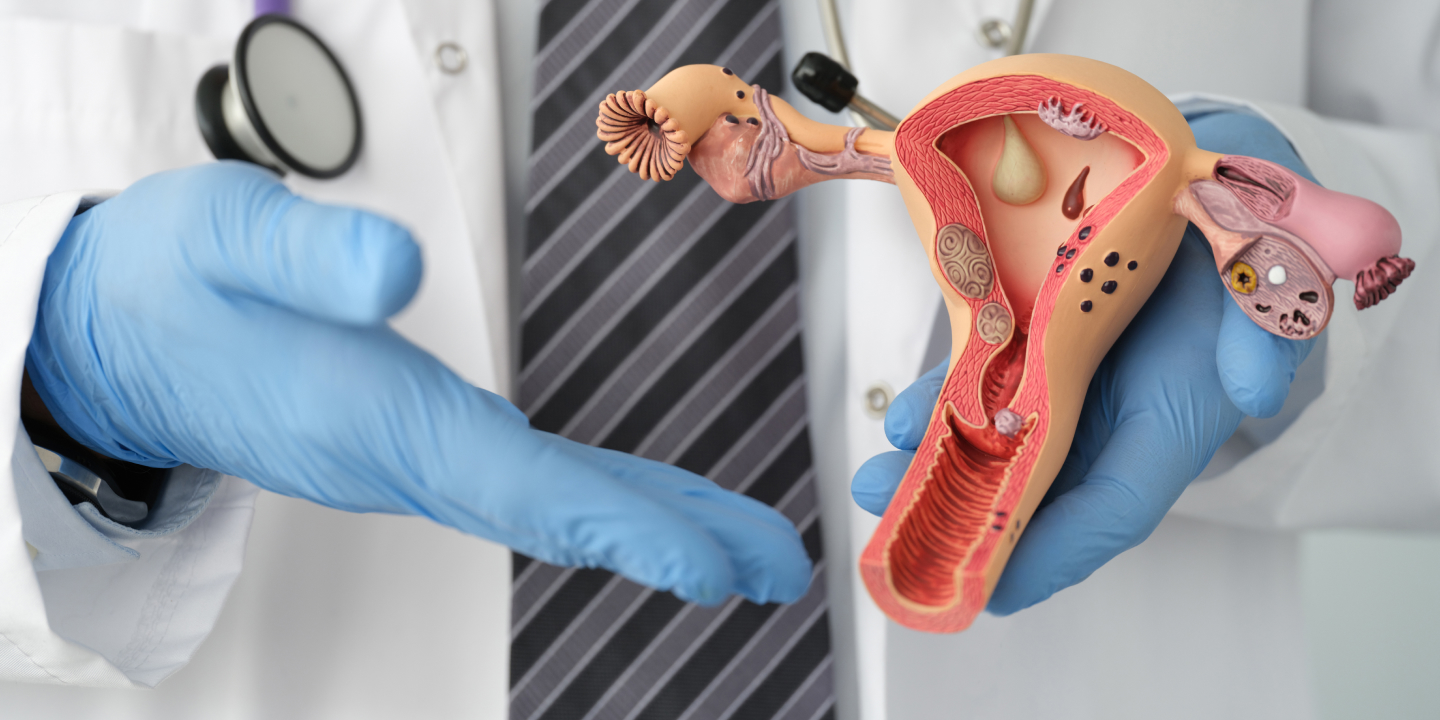
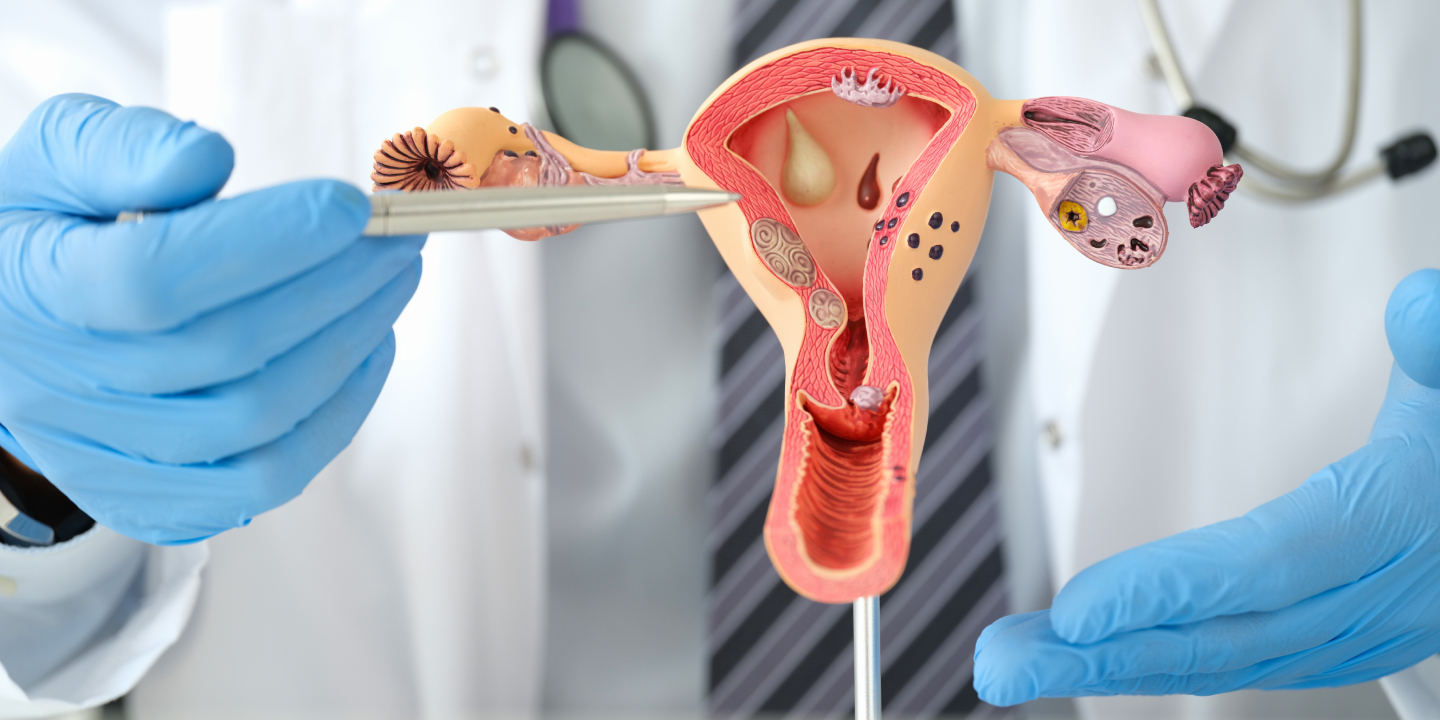
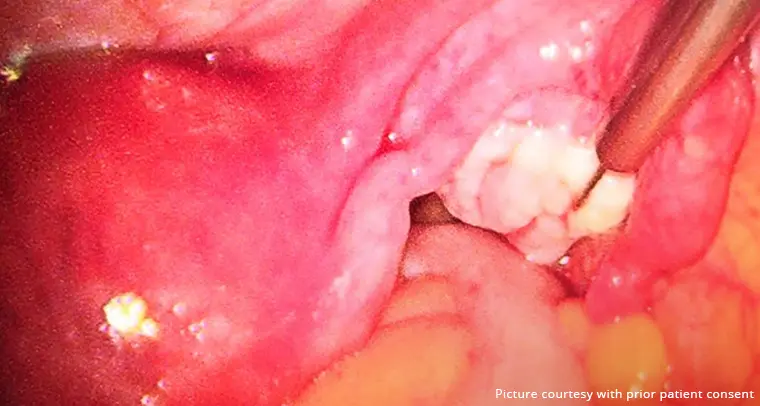
Once the initial consultation is over, the next step is to conduct a pelvic examination to examine the extent of the infection. The examination might be limited to the abdominal and pelvic region or involve examination of the external genitalia and/or the vagina too.
Comprehensive diagnosis might also involve taking a sample of the vaginal discharge to examine the type of fungal growth that is contributing to the symptoms.
Related Blog – Pelvic Pain During Pregnancy: Causes And Treatments
How is Genital Fungal Infection Treated?
At Queen’s Gynecology, the first step in genital mycotic infection treatment is a comprehensive and confirmed diagnosis. Following that, a tailored treatment plan is prescribed to the patient.
There are two primary routes of treatment available:
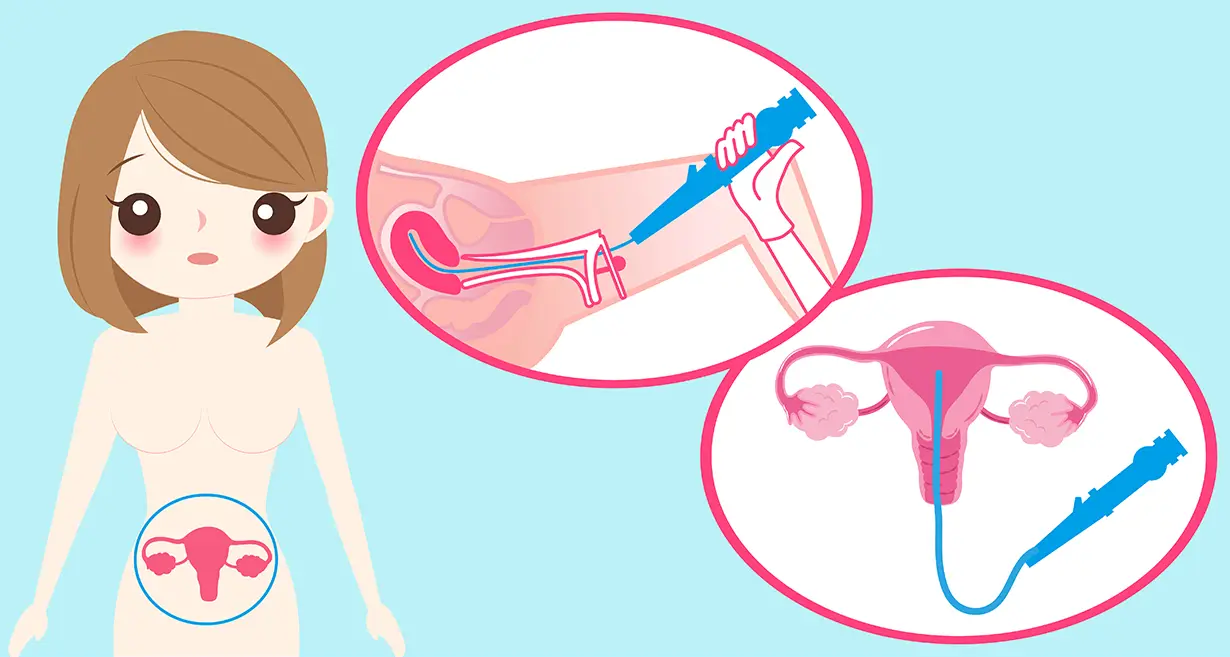
Topical creams or suppositories
If we suspect that the infection is in its early stages and is contained and hasn’t spread enough, the use of topical antifungal ointments and suppositories is considered an ideal and effective route of treatment.
The ointment is typically prescribed to be applied in the genital areas for a week. Although these medications are OTC, it is better to discuss their application with a gynecologist before buying them.
Oral antifungal medications
If the standard application of ointment and suppositories isn’t working, the next step is to opt for oral antifungal medications. The most common antifungal drug prescribed is fluconazole. A certified medical professional will prescribe the dosage.
Note: Patients that are struggling with recurring yeast infections are often treated under a maintenance plan. This prevents yeast overgrowth in the genitals and helps treat the condition for the better. Additionally, there are studies that indicate that genital fungal infections that are caused due to diabetes can be better cured using vaginal suppositories.
Are There Any Home Remedies that Help Treat Vaginal Yeast Infections?
Most women experiencing genital yeast infection due to diabetes often resort to using yogurt, oregano oil, coconut oil, and tea tree oil as a means to treat the condition.
However, kindly understand that these might not be effective in alleviating the symptoms. Relying solely on home remedies might lead to complications in the future.
What are some Preventive Measures for Genital Fungal Infection?
If you struggle with diabetes (type 1 or type 2), there is already an elevated risk of developing genital fungal infections. The last thing you want is to exacerbate it. One of the most effective preventive measures is to regulate your blood glucose levels.
Besides that, the following are some of the other preventive measures worth prioritizing:
- If you have a risk of contracting vaginal infections, avoid wearing tight-fitted clothes and undergarments that can make the genital area moist.
- Switch to wearing cotton underwear to regulate moisture levels.
- Avoid douching or intimate hygiene sprays available in the market.
- Ensure that you are prioritizing menstrual hygiene.
- Avoid using scented menstrual pads or tampons.
These are a handful of preventive measures that can help you overcome the risks of vaginal yeast infections, especially if you are a diabetic.
Related Blog – Endometriosis: Causes, Symptoms, Diagnosis & Treatment
Conclusion
The correlation between vaginal yeast infection and diabetes is unmatched. While it is true that unregulated blood sugar levels enhance the risks of an infection, it is also true that the risks are manageable with proper diabetes management, intimate hygiene, and a healthy lifestyle.
Vaginal infections should never be taken lightly. If you are experiencing uncomfortable symptoms, our specialist gynecologists at Queen’s Gynecology are here to guide you through the issue and offer effective treatment to ensure optimal quality of life.
Kindly contact us directly for appointments and related queries.
FAQs
In a 2019 study, the researchers concluded that diabetes patients are more likely to develop a vaginal yeast infection caused by the overgrowth of Candida glabrata.
Diabetes patients often have high blood glucose levels in their body along with a compromised immunity. Since yeast feeds on sugar, the excess sugar in the body along with poor immunity leads to overgrowth of the yeast, contributing to fungal infections.
The diabetes drugs that are categorized under “SGLT-2 inhibitors” are more prone to contributing to risks of genital fungal infections in diabetics. But, it is not a standard and is more of a subjective patient experience.