Risk content: Pelvic organ prolapse is a common condition in women that has a direct effect on their bladder control. The pelvic organs comprise of vagina, uterus, bladder, and bowel; the condition occurs when they sag and may bulge or protrude into the vagina. At an early stage, there are no signs of prolapse, but experts can see it during routine pap smear tests. The more a woman has vaginal births, they are more prone to have a prolapse. However, the condition may also be genetic and can run in families. It is best to consult an expert gynecologist to have a pelvic exam procedure if you experience symptoms of pelvic organ prolapse. Prolapse can be treated without any surgery in the early stages and when the prolapse is mild. QUEEN’S GYNECOLOGY is among the best clinics to get timely intervention for pelvic anomalies and to get on-time treatment.
In this Article
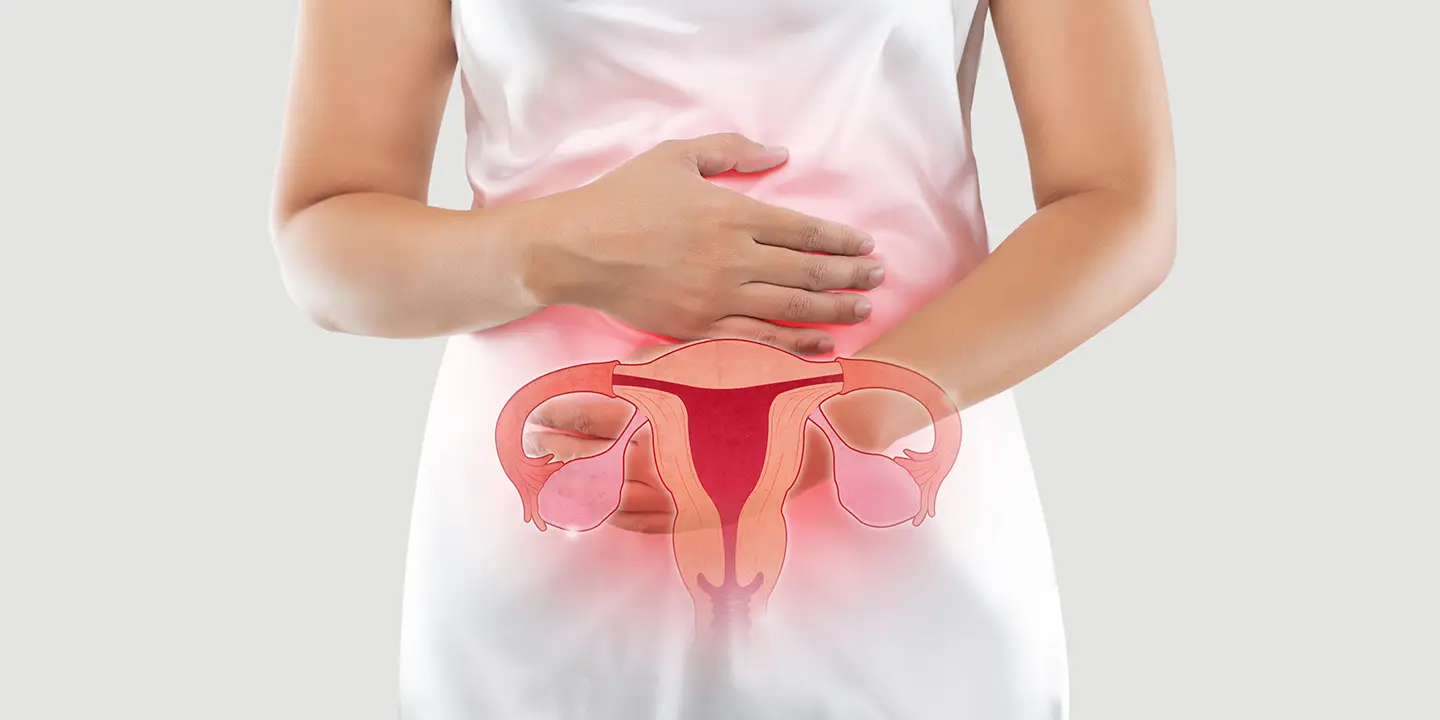
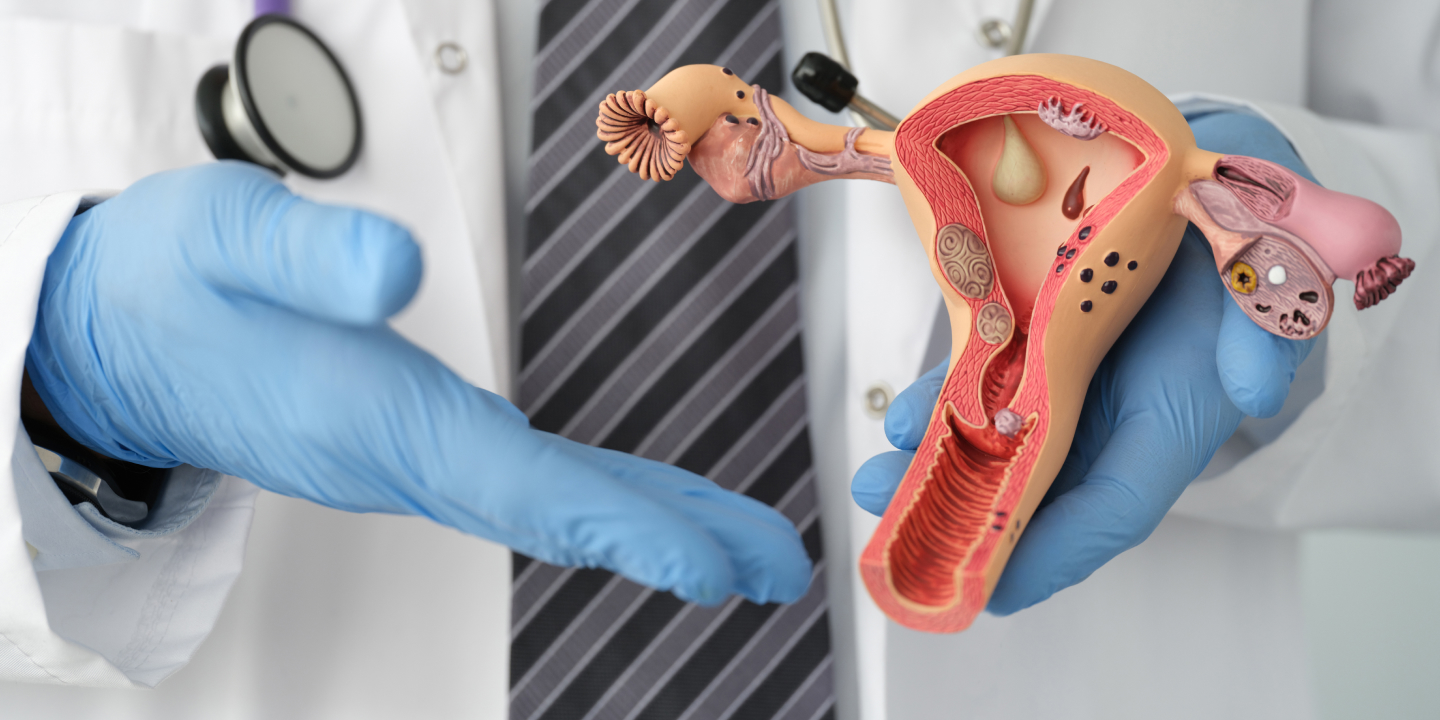
Pelvic organ prolapse – An overview
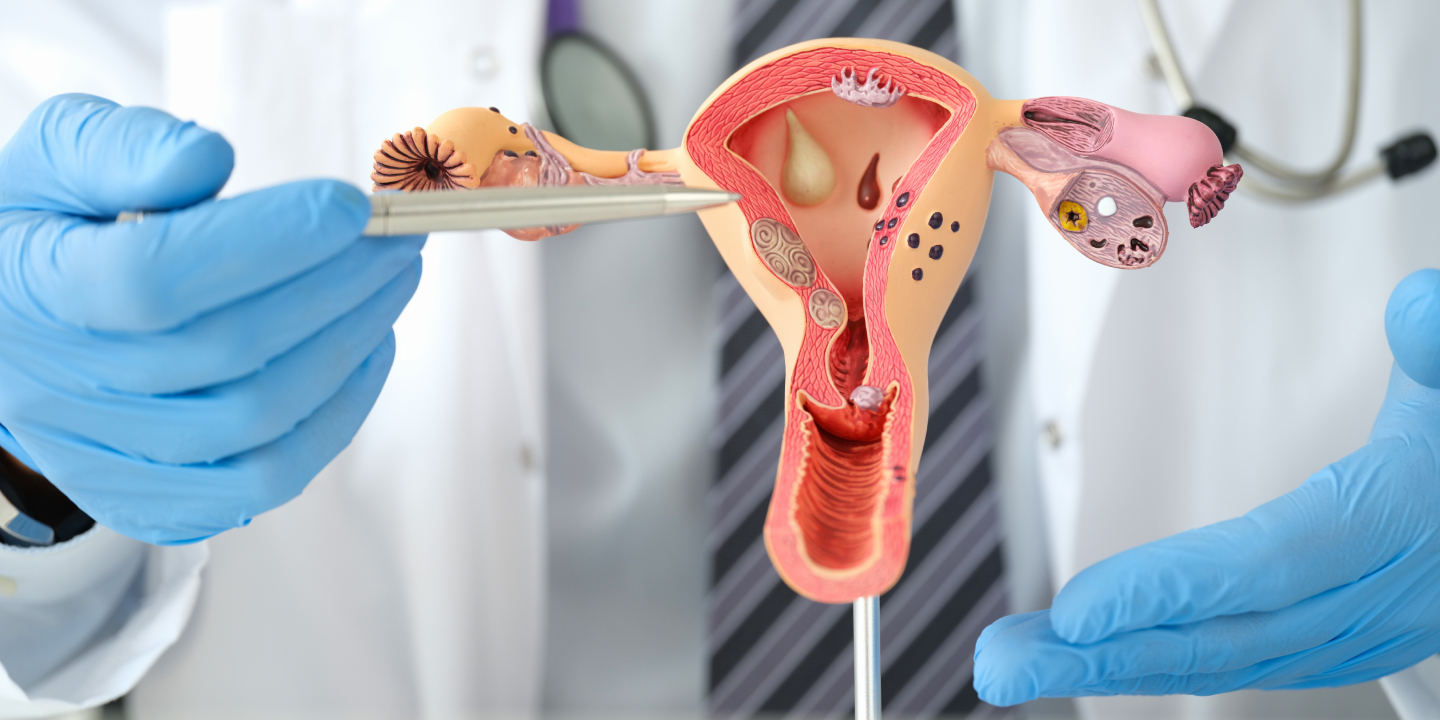
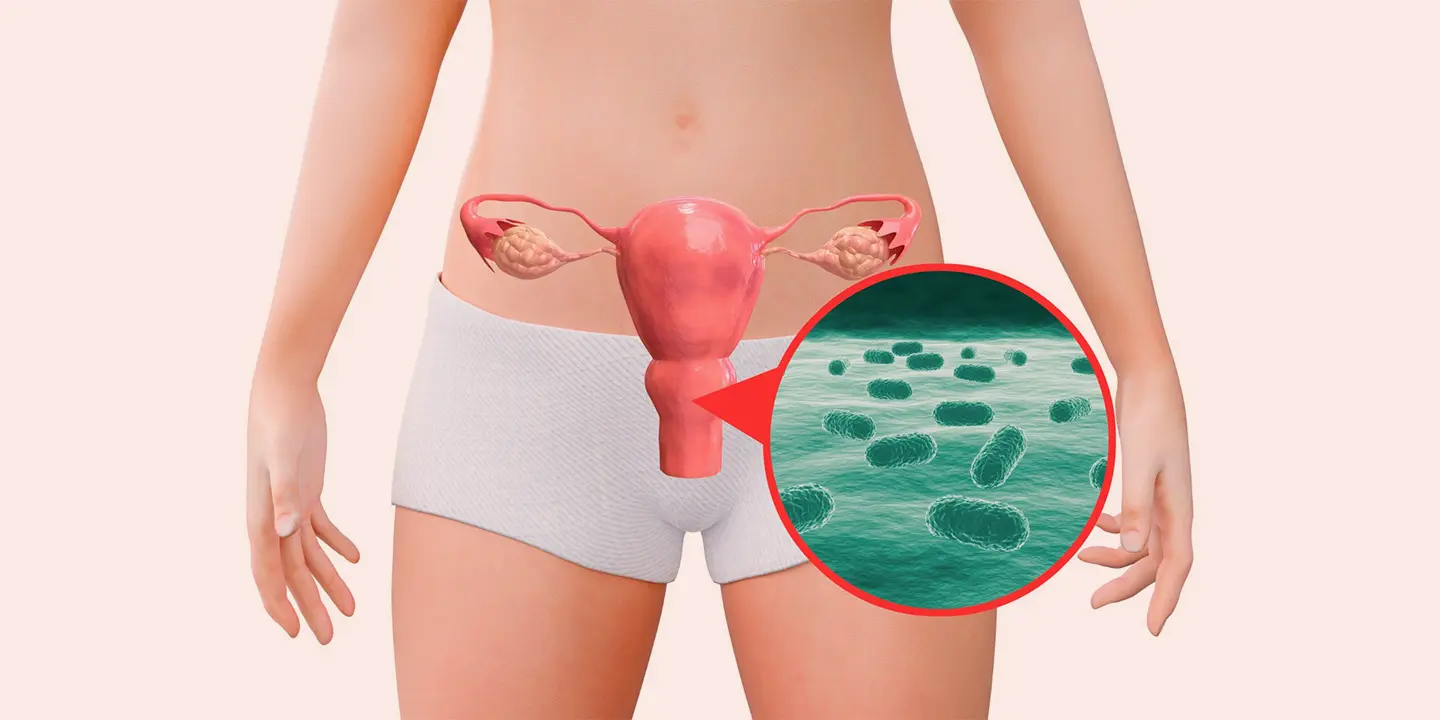
Pelvic organ prolapse is the dispositioning of pelvic organs from their normal positions in the pelvis. The pelvic structures that are associated are the uterus, vagina, cervix, bladder, urethra and rectum. Among all, the bladder is the most common organ that is involved in pelvic organ prolapse. The condition occurs when the tissue as well as muscles of the pelvic floor no longer support the pelvic organs, leading to a drop or prolapse of the organs from their normal positioning. A pelvic examination procedure done by an expert gynecologist can help you to diagnose it well and to get the appropriate treatment. Many women feel embarrassed to discuss the symptoms with the doctor, and some also think that symptoms are normal, but the prolapse is treatable and should be treated on time. There are types of pelvic organ prolapse :
- Posterior wall prolapse
This is also known as rectocele and enterocele, and it occurs because of loss of support to the back wall of the vagina. Because of loss of support, the intestines drop-down, and vaginal tissue may bulge. Symptoms include a bulge sensation, bowel movement issues, and the need to put a finger in or around the vagina to empty the bowel.
- Apical prolapse
It is also known as uterine prolapse or vaginal vault prolapse, which occurs when the supportive tissue of the cervix and uterus detaches from its attachment to the ligaments and muscles.
Related Blog: Pelvic Floor Dysfunction: Symptoms, Causes & Treatment
- Rectal prolapse
In some cases, the supporting structures in the electrum detach from the wall, and the organ comes out through the anus. Symptoms comprise pain during bowel movements, mucus or bowel discharge, and loss of control of bowel movements.
Common symptoms of pelvic organ prolapse
POP occurs when pelvic organs drop from their original positions in the pelvis. It can be detected through a pelvic test, and the condition is very common in older women. Some symptoms are:
- Dragging feeling in lower abdomen and pelvis.
- A feeling of swelling in the vagina or a lump outside vagina.
- Backache that gets severe day by day
- Vaaginal bleeding and discharge
- A problem in passing urine or stools
- Problem in or inability to have intercourse
- Problem with sitting or walking
Pelvic organ prolapse – main causes
Pelvic organ prolapse occurs when the attached tissues or muscles of the pelvis do not work as they have to and detach / Some common causes of the condition are :
- Vaginal birth – it is a common cause that stretches and puts a string on the pelvic floor. Vagainal childbirth increases your risk and makes you more prone to prolapse of organs.
- Long-term pressure of the abdomen- the condition also occurs due to pressure because of obesity, chronic coughing, etc.
- Delivery of healthy baby – Giving birth to a baby weighing more than 8 pounds
- Aging – is also a factor, as older women are more prone to POP.
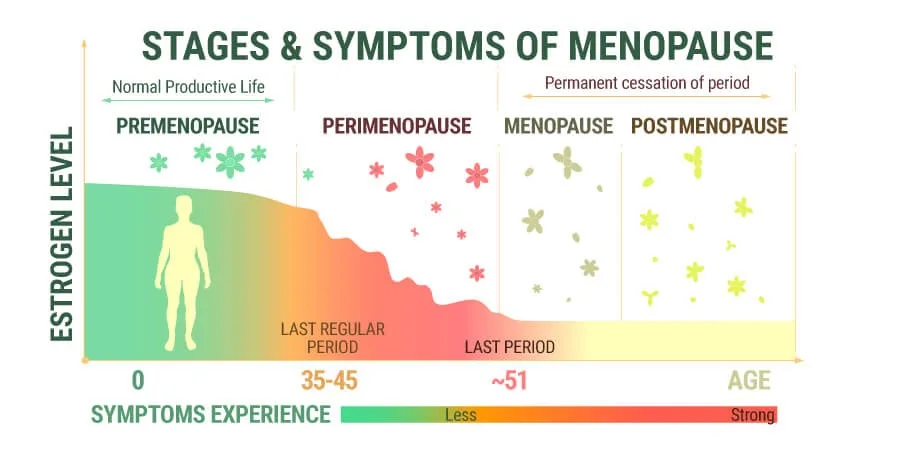
- Hormonal changes – loss of estrogen during or post menopause can increase your risk.
- Family history- the condition also runs in families.
Pelvic organ prolapse – Treatment options
If you experience any symptoms of pelvic floor prolapse, then you have to undergo a gynecological exam. Your gynecologist may also do other tests to see whether these actions cause prolapse or urine leakage. During your appointment, your gynecologist will check and review your symptoms and perform a pelvic exam. During this exam, they will ask you to cough and see the extent of your prolapse. They may recommend bladder function tests like cystoscopy and urodynamics tests along with imaging tests to view inside your pelvic cavity. To treat pelvic organ prolapse, your gynecologist is strict with nonsurgical first-line treatments, and if these treatments do not work, they may recommend surgery. Some nonsurgical and surgical treatment options to treat pelvic organ prolapse are :
Nonsurgical options :
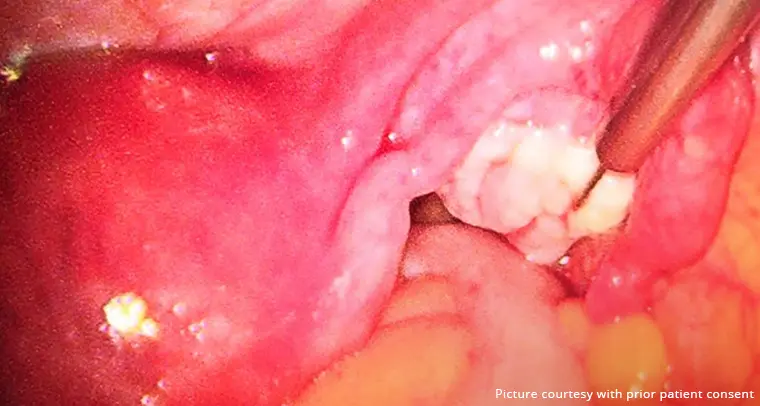
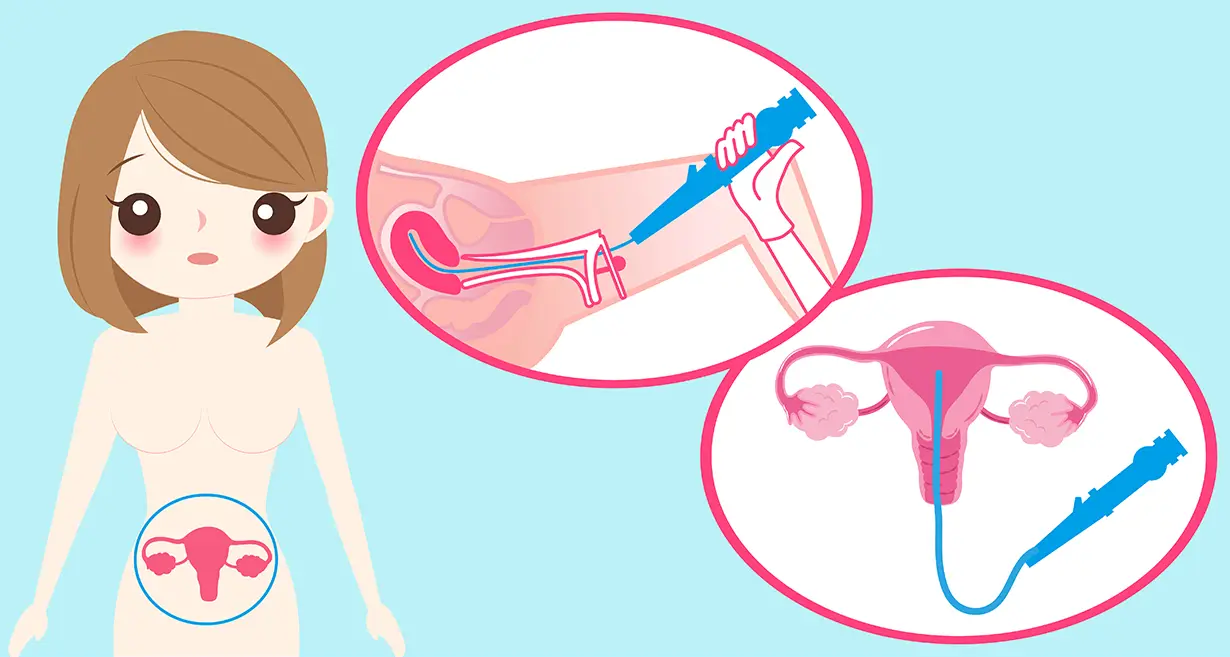
- Vaginal pessary – a device that the doctor will insert into your vagina to put your organ in place.
- Pelvic floor exercises – also termed as kegel exercises to strengthen the pelvic floor. They may also recommend a physical therapist to teach you targeted exercises.
Related Blog: Pelvic Inflammatory Disease (PID): Symptoms & Treatment
Surgical options:
Surgical treatment options may also be recommended if symptoms do not improve with nonsurgical options and if you no longer need to have children. Two types of surgeries are obliterative and reconstructive surgery. The former surgery option is to sew vaginal walls that prevent organs from slipping, and the latter option repairs the weakened parts of the pelvic floor. Types of surgery are :
- Copaclesis
- Colporrhaphy
- Sacrocolpopexy
- Sacrohysteropexy
- Uterosacral or sacrospinous ligament fixation
How Queen’s Gynecology can help you with pelvic and uterine anomalies?
Many uterine and pelvic anomalies may lead to many issues like pelvic organ prolapse (POP), which doesn’t get talked about much because women feel shame or are confused about the condition or its treatments. Women need to discuss and work with a pelvic floor specialist to get a proper cervical exam and to start the treatment according to their needs and wishes. At Queen’s Gynecology, an expert team of doctors will help you with any type of women’s health issues, including pelvic organ prolapse. The expert may recommend nonsurgical treatment of pelvic organ prolapse, comprising the use of pessary and pelvic floor exercises, and can also help you with surgical options that are best for you if needed. Grounding your expectations in honest conversations with gynecologists at the best clinic in Delhi will improve your experience with the condition. The main aim of experts here is to identify any anomalies using the latest modalities and correct them on time. If you are experiencing the symptoms of pelvic organ prolapse, then they will monitor your prolapse and recommend treatments if it progresses and negatively impacts your quality of life.
Conclusion
Pelvic organ prolapse is a common but serious condition if left untreated, can harm your body image and your sexuality. Never feel embarrassed to talk to your gynecologist if you have the symptoms or you suspect a weakened pelvic floor during a gynecological exam. Keep in mind that your pelvic floor health is as vital as your overall health and is an important part of your well-being. Together with an expert ob-gyn at QUEEN’s GYNECOLOGY, you can give your pelvic floor the needed attention and proper care that you require.
FAQ’s
The bladder is the most common organ to prolapse. The condition when that happens is called cystocele.
Many women recover well and feel better post-surgery as it allows them to get into the routine of their normal activities.
The prolapse may come back after surgery as some factors make you more prone to repeated prolapse, including the factors of you being overweight or younger than 60 years.