Birth control comes in various shapes, purposes, and sizes. Among them, Mirena is a name that often pops up here and there. For those who are completely clueless, Mirena is a hormonal contraception method.
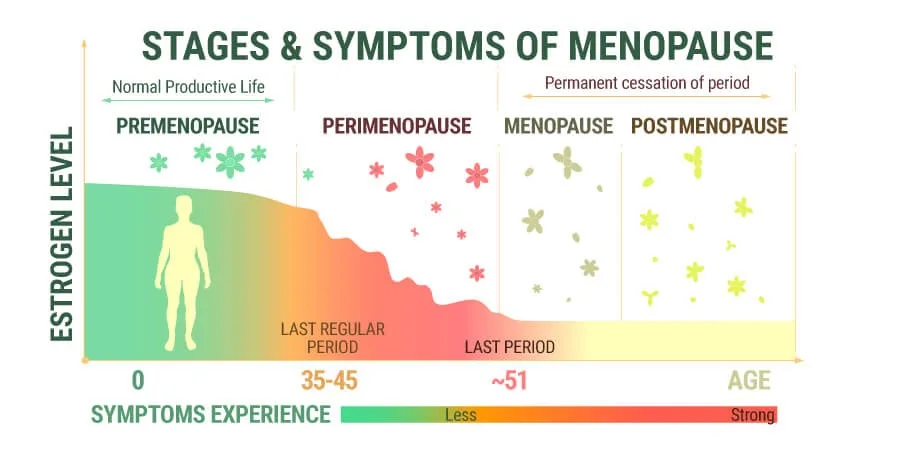
Perimenopause is a transitional phase in a woman’s life that typically occurs in her late 30s to early 50s, leading to menopause. During this time, hormonal fluctuations can cause various physical and emotional changes, including irregular menstrual cycles, hot flashes, mood swings, and other menopausal symptoms.
Mirena has been found to have amazing benefits for alleviating those symptoms and enabling perimenopausal women to have a better quality of life. This article will explore everything about Perimenopause, Mirena, and its effects.
In this Article
- 1 What is Perimenopause?
- 2 Mirena: A Brief Overview
- 3 How Effective is Mirena as a Contraceptive During Perimenopause?
- 4 What are the advantages of Mirena during Perimenopause?
- 5 How long should a mirena coil be inside the uterus?
- 6 What are some considerations before Choosing Mirena?
- 7 Does mirena coil affect the onset of Menopause?
- 8 Conclusion
What is Perimenopause?
Perimenopause is the phase in a woman’s life, especially between the ages of 30 and 50, when reproductive hormones decline gradually. This leads to complications like irregular periods, heavy bleeding, and the associated symptoms of menopause.
In most cases, women experience 4–10 years of perimenopause before they hit the menopause phase.
The symptoms of perimenopause are diverse, including:
- Heavy bleeding during periods
- Hot flashes
- Night sweats
- Mood swings
- Vaginal dryness
- Changes in menstrual patterns, etc.
These symptoms, albeit big or small, significantly impact a woman’s quality of life in the long run.
Mirena: A Brief Overview
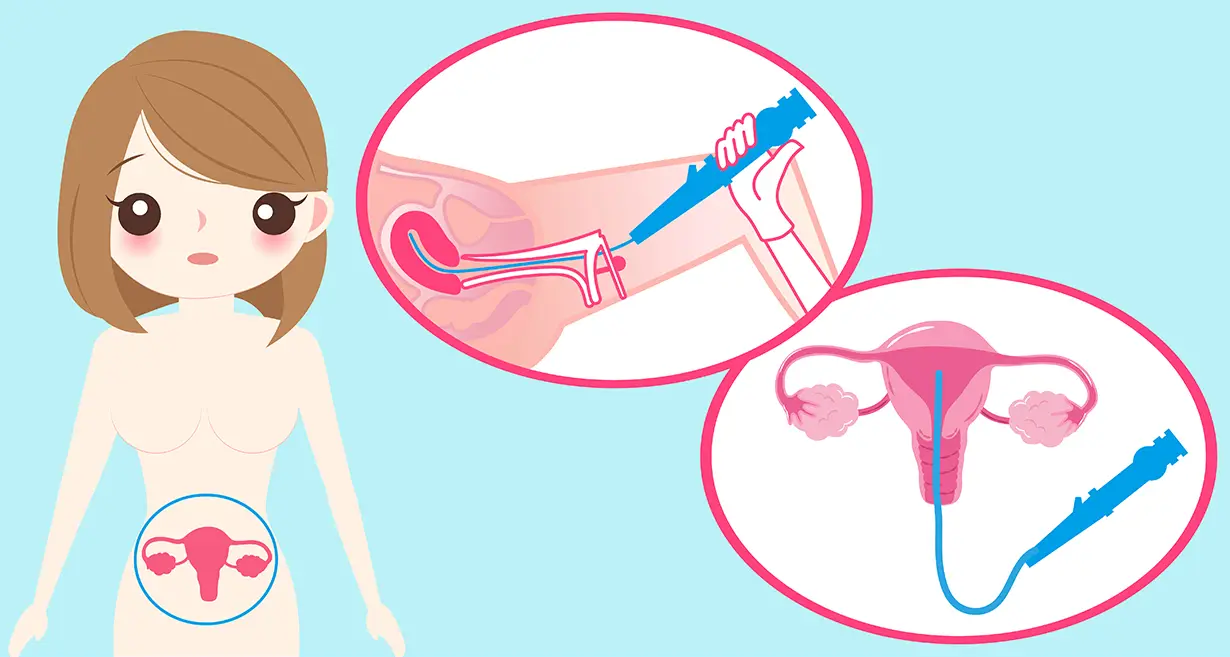
Mirena is a type of contraception. Let’s start with that. The follow-up question is, “What kind of contraception is it?” The Mirena coil is a hormonal IUD that has beneficial impacts on preventing pregnancy risks in perimenopausal women.
What’s unique about this form of birth control or contraception and its impact? Mirena isn’t just for avoiding pregnancy. Instead, it works for symptom management too. For example, it helps prevent the risk of heavy bleeding during periods.
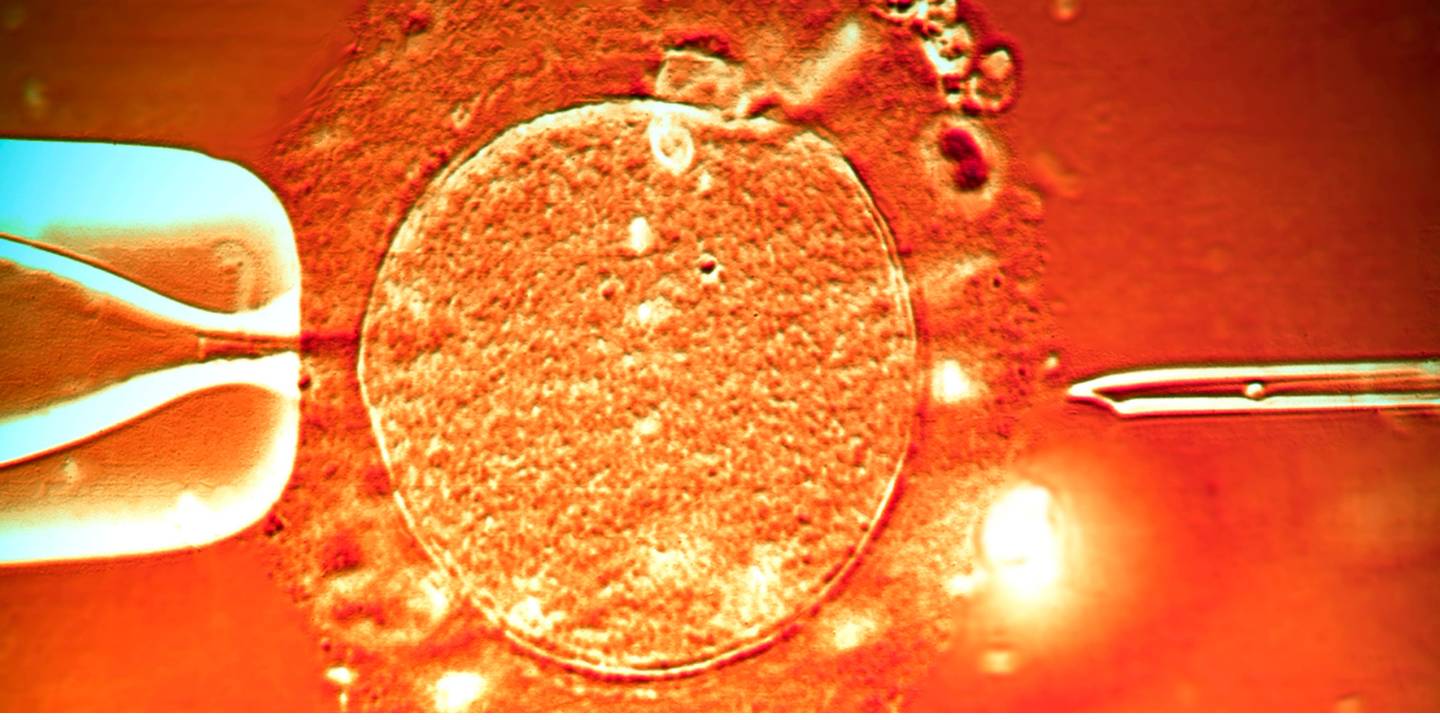
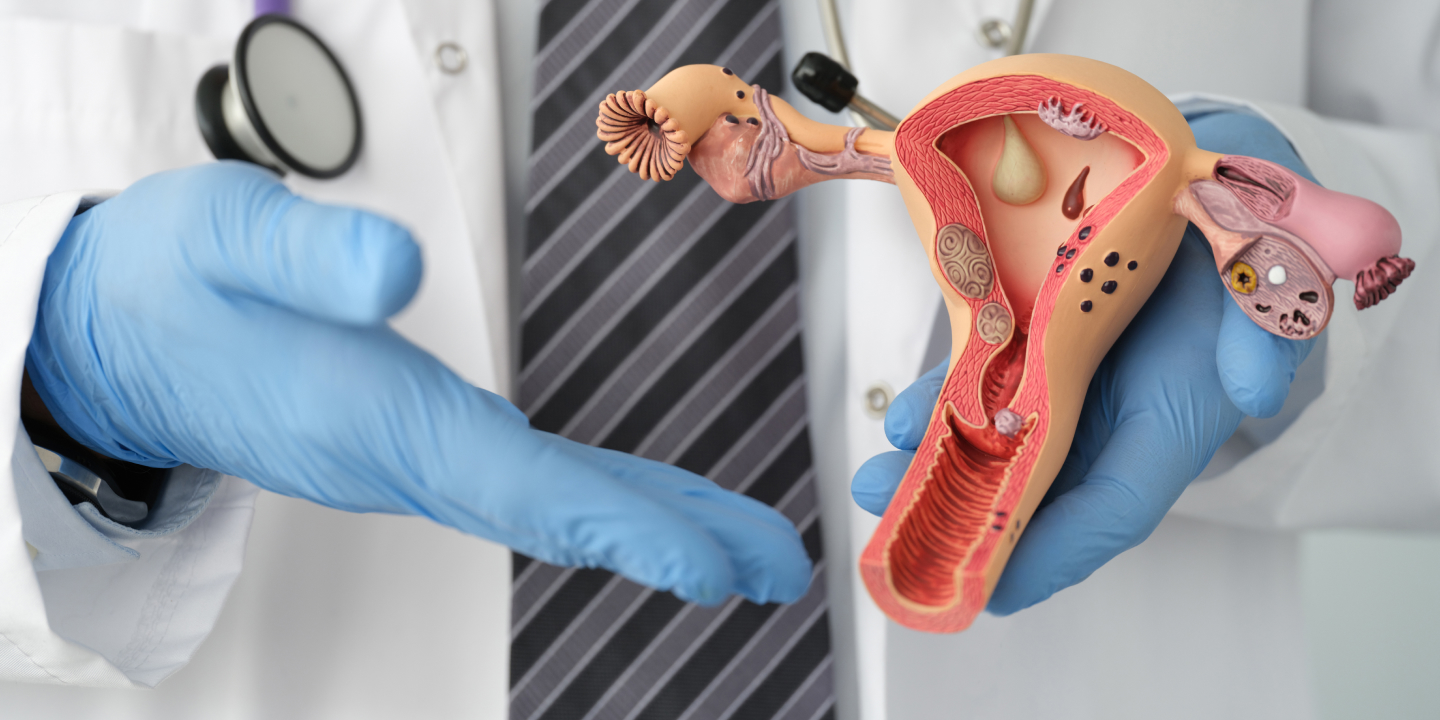
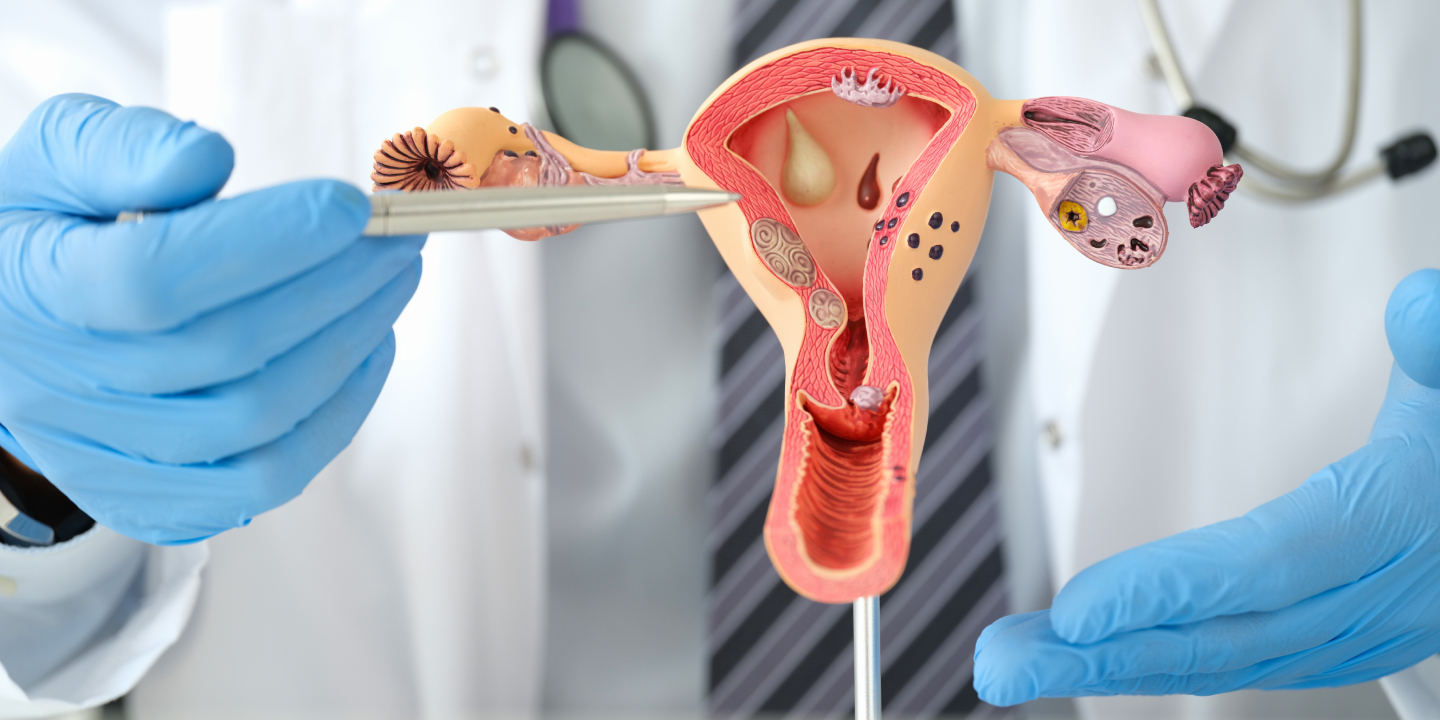
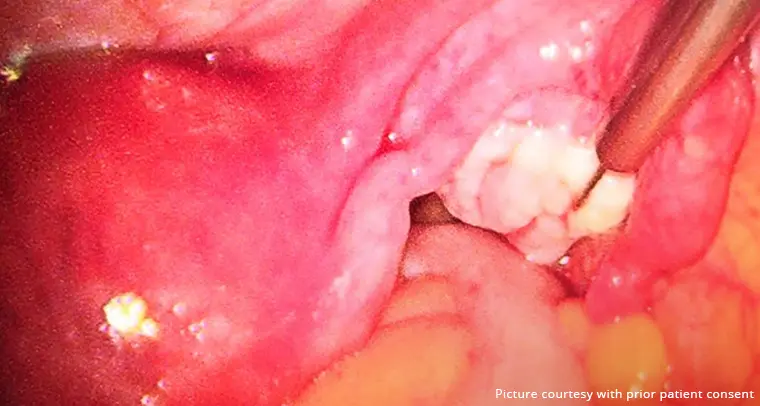
When we get into the scientific or medical side of things, the Mirena coil is a T-shaped coil containing levonorgestrel, a synthetic form of the hormone progesterone. It is inserted into the patient’s uterus by a medical professional.
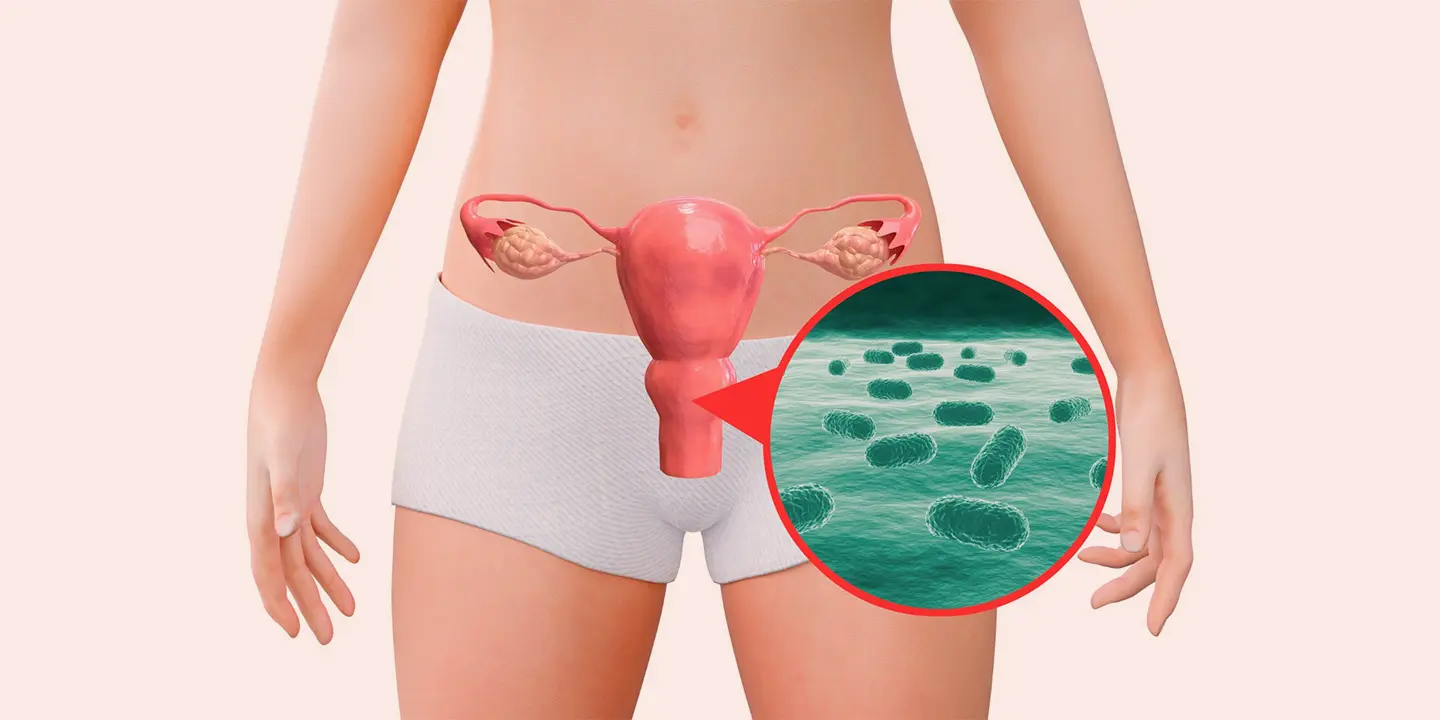
Once inserted into the uterus, the IUD releases a low dose of levonorgestrel into the uterus, thereby thickening the cervical mucus. What this does is prevent the sperm from reaching the egg, preventing fertilization and eventually pregnancy too.
How Effective is Mirena as a Contraceptive During Perimenopause?
Perimenopause can start anywhere between 30 and 50 years old in women. This is considered the average age range and can vary from one woman to another.
One of the most common misconceptions people have is that perimenopause automatically means that a woman won’t conceive if she is engaging in unprotected sex. That is simply not true.
While it is true that a woman’s reproductive health and fertility start to decline as she hits perimenopause, that doesn’t mean she can’t get pregnant during that period. This is one of the reasons why using some kind of birth control is mandatory if one doesn’t want to get pregnant.
Until one hits menopause (hasn’t gotten the period for 12+ months), there are chances that one can get pregnant if they engage in unprotected sex.
Since the Mirena coil is a hormonal contraception method, it releases levonorgestrel, further preventing the risks of pregnancy in perimenopausal women.
What are the advantages of Mirena during Perimenopause?
If you are looking for the best IUD for perimenopause, the Mirena coil is undoubtedly available.
Let us walk you through the list of benefits:
1. Highly Effective Contraception
Mirena stands out as one of the most effective forms of female contraception. It has a failure rate of 1%, which means that you have a very slim chance of getting into the fuss of unwanted pregnancies.
This aspect is especially crucial for women in the perimenopausal phase who may still be sexually active but desire to avoid conceiving for various reasons, such as health concerns or life circumstances.
Furthermore, Mirena offers a long-term contraceptive solution, which means one won’t have to worry about it daily. Once the Mirena coil is inserted into the uterus, it remains effective for up to five years. This means you won’t have to worry about taking pills every day or forgetting them.
2. Regulation of Menstrual Cycles
Perimenopause brings a lot of challenges for women, especially regarding their menstrual cycles and the symptoms that come with them.
This phase in a woman’s life is marked by rigorous hormonal fluctuations, which often contribute to irregular periods and heavy bleeding. Mirena’s ability to regulate menstrual cycles provides a sense of predictability and control over this aspect of a woman’s life.
Mirena also leads to lighter and less frequent periods in women, ensuring optimal quality of life for them. Having more manageable and predictable periods can increase confidence and freedom to engage in daily activities without fearing sudden, heavy bleeding.
3. Management of Menopausal Symptoms
We are primarily focused on Mirena and perimenopausal symptoms, but we had to include this in the list of benefits. One of the most notable symptoms that Mirena can address is heavy menstrual bleeding, also known as menorrhagia, which is relatively common during perimenopause.
Beyond managing heavy bleeding, Mirena may also offer relief from other menopausal symptoms, such as pelvic pain and cramping.
Mirena provides perimenopausal women with an array of advantages, making it a compelling choice for hormonal contraception and symptom management.
How long should a mirena coil be inside the uterus?
On average, an inserted Mirena coil in the uterus can last for about 5 years and remain effective throughout that period.
However, you need to understand that there is no “set time” or “standard” time to remove the Mirena coil. It is generally removed once it expires.
At Queen’s Gynecology, we always advise our patients to understand the pros and cons of contraception, ensuring that they have comprehensive knowledge about it before undergoing the procedure.
What are some considerations before Choosing Mirena?
As you are reading through the “Mirena for perimenopause reviews,” there are certain factors that you have to keep in mind.
Since Mirena is a form of hormonal contraception, there are a variety of factors that one needs to weigh before deciding if it’s the ideal form of contraception for them.
Following are a few considerations worth looking into:
1. Suitability and Medical History
Before you opt for the Mirena coil during your perimenopause, women must discuss their medical, reproductive, and sexual histories with their individual healthcare professionals.
Our patients at Queen’s Gynecology who consider getting Mirena always undergo a thorough medical evaluation and consultation before the procedure.
For example, patients suffering from uterine complications and pelvic inflammatory disease aren’t ideal candidates for this form of contraception.
2. Potential Side Effects
Like most forms of contraception, even IUD Mirena side effects should be paid close attention to. Experiencing the side effects isn’t as extensive and is quite rare.
However, albeit rare, some side effects include headaches, irregular bleeding during periods, mood swings, breast changes, etc. The symptoms are often temporary or short-lived and will disappear as the body adjusts to the contraception.
3. Insertion and Removal Procedure
Patient education is an integral part of our practice at Queen’s Gynecology. Before performing any procedure, we always aim to discuss the treatment details with the patient at length.
This includes breaking down each and every step of the procedure and weighing out the pros and cons. Mirena coil insertion in the uterus is a safe procedure and only takes a few minutes. However, our priority is the optimal comfort of the patient. Hence, being aware of the steps is crucial.
The Mirena IUD is undoubtedly one of the most effective forms of contraception for perimenopausal women. However, it isn’t the only one. Hence, weighing the pros and cons is crucial before the device is implanted.
Does mirena coil affect the onset of Menopause?
Mirena is a type of contraception, which means that it’s needed by fertile women who can get pregnant. It is not a necessity once you hit menopause.
That said, one of the most common myths is that the Mirena coil affects the onset of menopause in women, which is simply not true.
One of the main modes of action of the Mirena IUD is that it suppresses ovulation in the patient. So, you don’t ovulate and have more eggs in the ovarian reserve, and your menopause is prolonged? Well, that’s not true.
Even when you aren’t ovulating, you lose ovarian follicles as you age. This means that despite the lack or reduced frequency of ovulation due to Mirena, it doesn’t affect the natural onset of menopause in the patient.
Conclusion
Mirena is an excellent option for perimenopausal women seeking effective contraception and relief from menopausal symptoms. If you were confused about it, we hope this article gives you a comprehensive rundown of all the integral factors involved.
Getting a comprehensive evaluation before a Mirena insertion is mandatory. Our team of experienced gynecologists at Queen’s Gynecology is here to guide you through the process, assess whether you are the right candidate, and offer comprehensive care before, during, and after the insertion.
For appointment-related queries, kindly contact us directly at +91 9654999888.