It is normal to experience some pelvic pain throughout pregnancy. After all, in order to create room for your expanding uterus, your ligaments are stretching, your hormone levels are altering, and your organs are rearranging. However, prolonged discomfort occasionally may be a sign of a more serious problem. Let’s read about how to identify your pregnancy-related pelvic pain, how to treat it, and when to seek medical attention.
In this Article
Causes Of Pelvic Pain During Pregnancy
People may suffer pelvic pain and discomfort during pregnancy for a variety of causes, including loosened pelvic joints and pressure from the weight of their growing baby. The most frequent causes of benign pelvic pain during pregnancy are listed below:
Symphysis Pubis Dysfunction (SPD)
The symphysis pubis, a joint in front of your pelvis, can become unstable during pregnancy and hurt your pelvic bones. It may begin soon after conception and develop worse as the pregnancy progresses.
SPD, also known as pelvic girdle discomfort, develops during pregnancy as levels of relaxin, progesterone, and estrogen rise. The ligaments in the pelvic region grow tender and become relaxed as the hormone levels increase, and the joints begin to move more readily.
Adaptation Pain
It can feel like you’re getting your period when you have this cramp-like pelvic pain, which typically starts 8 to 12 weeks into your pregnancy. Compared to later pregnancies, your first pregnancy has a lower likelihood of you experiencing this.
Round Ligament Pain
You might experience a severe, stabbing, or agonizing pain in your side, close to your pelvis, in the second trimester. The ligament connecting the uterus to your groin may become stretched as a result of your baby’s growth.
Additionally, the pain in your round ligaments may worsen when you move. The uterus tilts and pulls on the ligament, for instance, when you walk or get up from a chair. You can relieve the discomfort by lying on the side that is hurting you (or alternate sides if both suffer). By 24 weeks, the majority of round ligament pain is gone.
Diastasis Recti
Extremely prevalent during and after pregnancy, diastasis recti can occasionally resemble pelvic pain brought on by SPD. The issue, which can result in a tummy bulge, happens when your rectus abdominis muscles split.
Your pubic bone is where the muscles of your lower abdomen attach, and hormonal fluctuations cause the pubic muscles to stretch. Your doctor may recommend an exercise regimen if you experience diastasis recti that don’t go away after your baby is delivered; more severe cases can necessitate surgery.
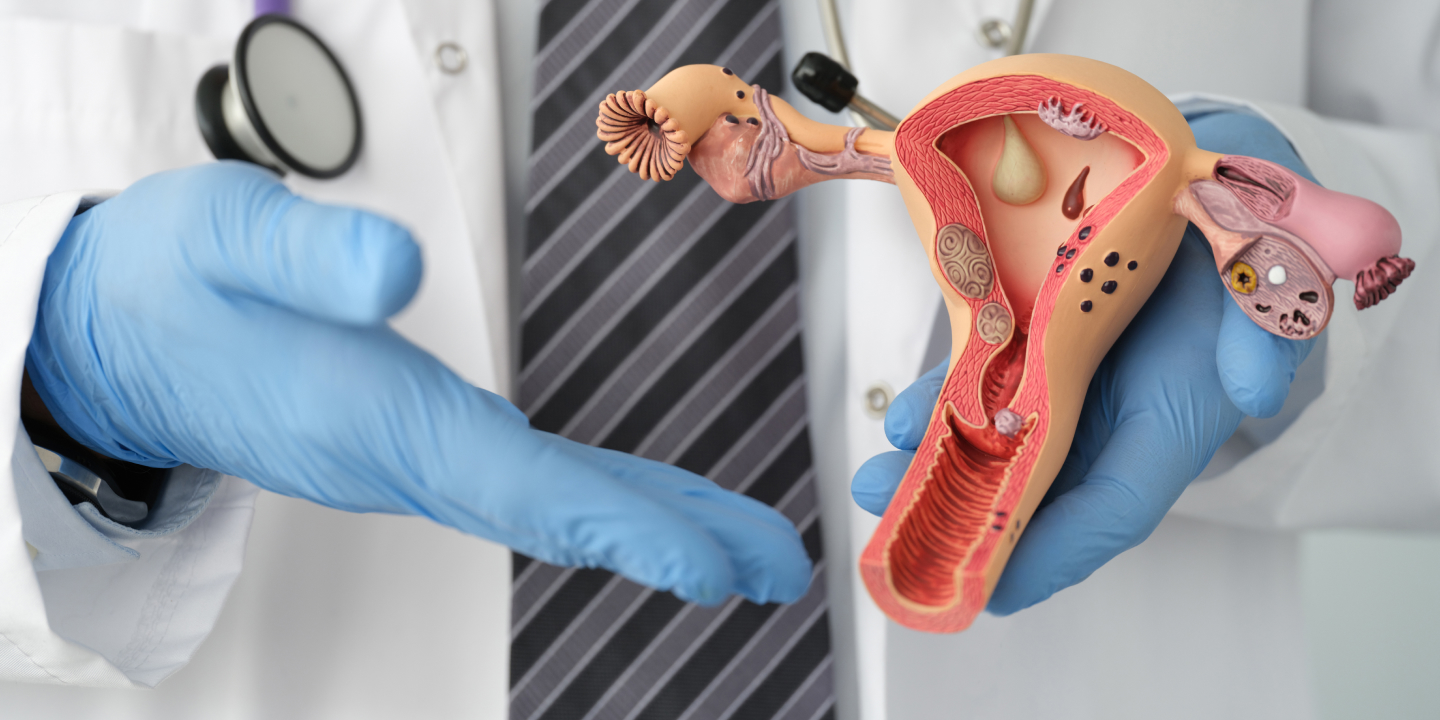
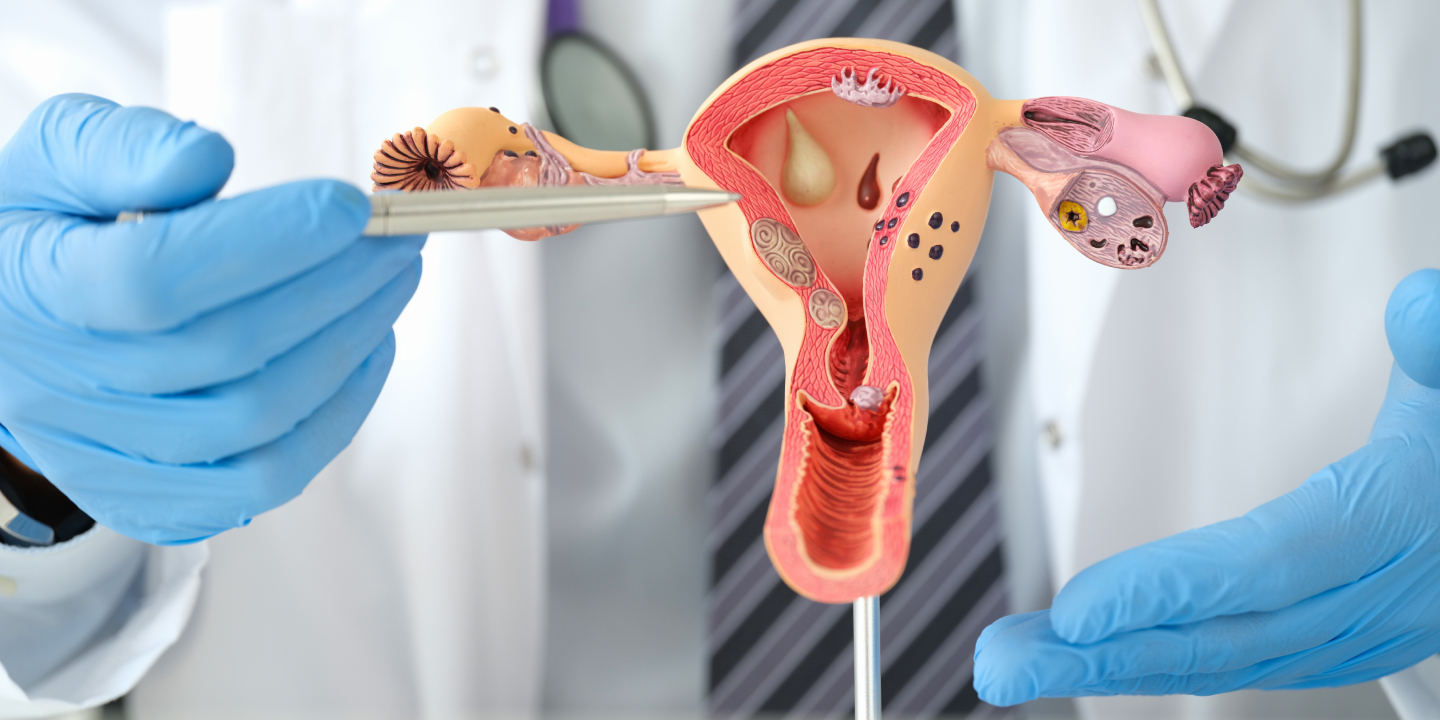
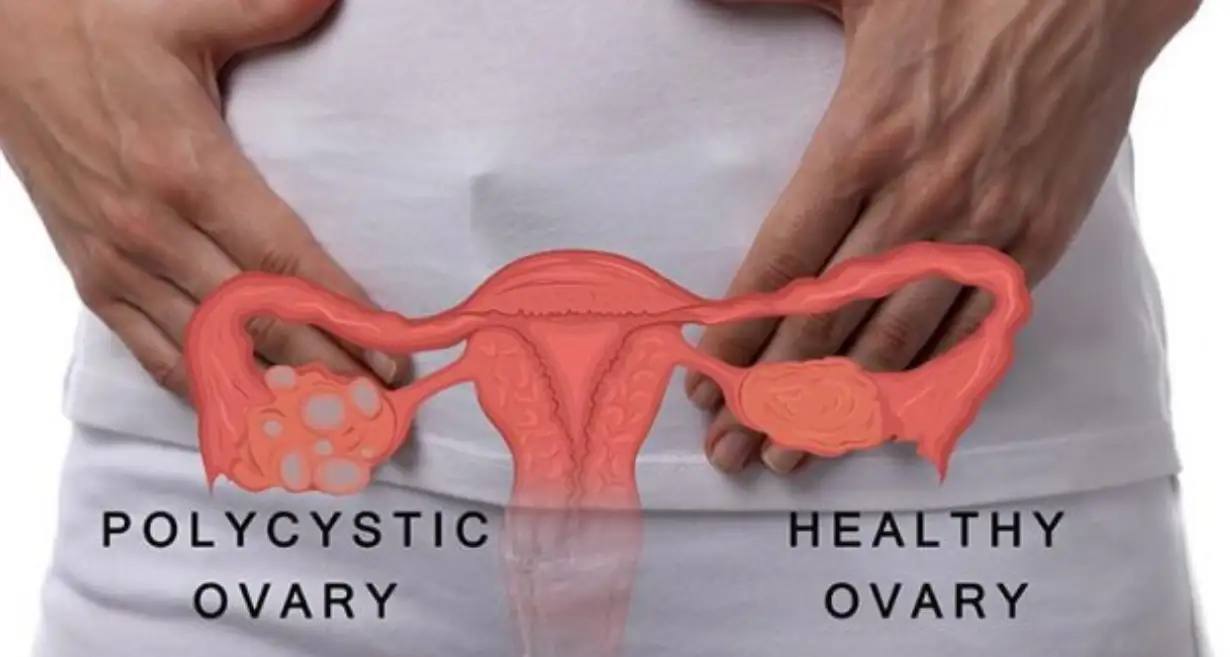
Ovarian Cysts
Pregnancy can cause ovarian cysts to grow and develop, which can cause pelvic pain in part because the expanding uterus exerts pressure on the ovaries. Cysts arise when your ovaries produce or release eggs differently. They are widespread, benign, and usually unharmful. If you have ever had cysts or believe you do, let your OB-GYN know. They can be located with an ultrasound.
Braxton Hicks Contractions
These so-called “practice contractions” typically feel like pelvic pressure or tightening and occur less frequently than labor contractions. Dehydration can cause Braxton Hicks, which first appears in the second or third trimester. Therefore, drink plenty of water. If you experience more than four contractions per hour for two hours, call your doctor since you might actually be in labor. Otherwise, they should go away on their own.
Urinary Tract Infection (UTI)
Having a UTI during pregnancy might cause you to have an intense urge to urinate, as well as a burning feeling when urinating and possibly some blood in your urine. Some folks also experience stomach aches. The main distinction is that during pregnancy, untreated infections can lead to major problems for both you and your unborn child.
UTIs during pregnancy can sometimes develop into kidney infections, which raise the possibility of preterm labor. One of the reasons your OB-GYN checks your urine at every appointment is to look for bacteria that can cause a UTI. The infection is simple to treat with medication if discovered early.
Related Blog – 10 Causes Of Pelvic Pain During Pregnancy, When Should Consult With Doctor
Severe Causes Of Pelvic Pain During Pregnancy
Pregnancy-related pelvic pain can occasionally be very severe. Call your doctor right away if your discomfort is accompanied by certain symptoms, such as bleeding or fever. These are some important reasons why pelvic pain might occur during pregnancy.
Miscarriage
You must constantly worry about miscarriage when a first-trimester sufferer complains of abdominal or pelvic pain. Up to 10% of known pregnancies and up to 26% of all pregnancies are thought to result in miscarriage. Bleeding and cramping, which may be rhythmic or mirror menstrual cramps, are signs of a miscarriage.
Preterm Labor
You might be in labor if you have a constant backache and intermittent waves of pelvic pressure. You should be examined if you experience four or more contractions per hour and they last for longer than two hours despite having urinated and lay down. It’s thought that having these symptoms before the 37th week of pregnancy may indicate preterm labor.
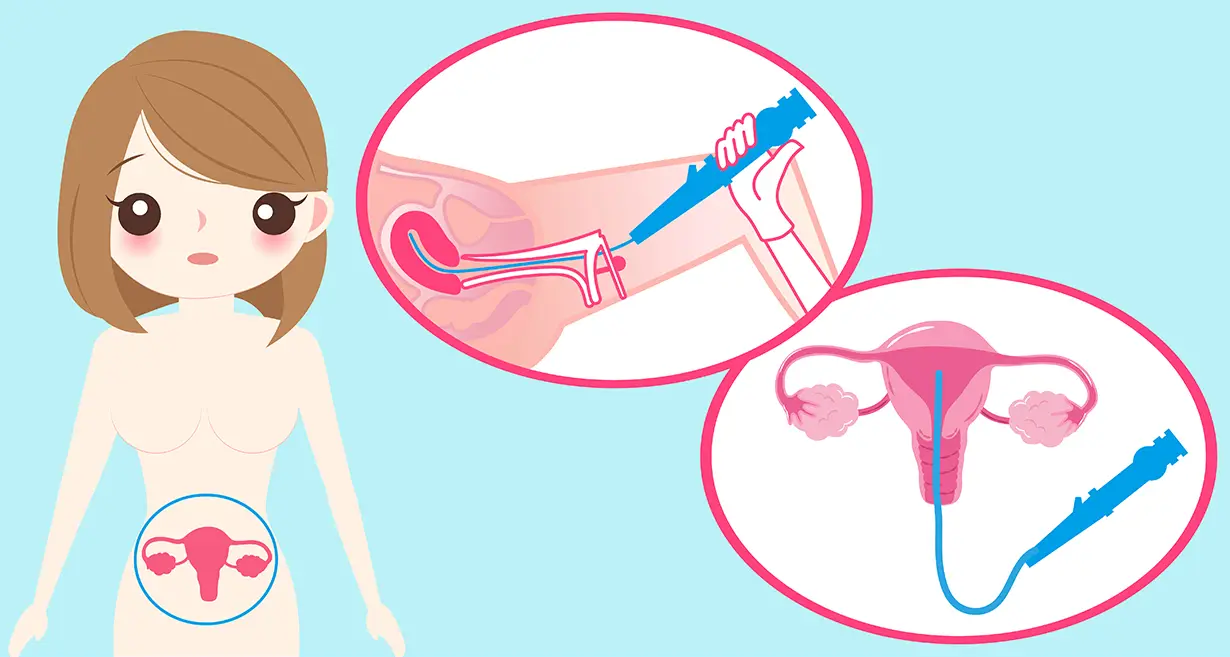
Ectopic Pregnancy
If you have an ectopic pregnancy, which is extremely unusual, you may have severe pelvic pain and bleeding between weeks six and ten of pregnancy as the tube swells. When a fertilized egg implants anywhere other than the uterus—typically in the fallopian tube—this is known as an ectopic or “tubal” pregnancy. In 1% to 2% of pregnancies, this can occur.
Ectopic pregnancies are more common in people who have already experienced one. Endometriosis, tubal ligations, pelvic infections, previous pelvic, abdominal, or fallopian tube surgeries, as well as the use of an intrauterine device (IUD) at the time of conception, all carry a higher risk. Anyone who used artificial reproductive methods to get pregnant as well as those with an irregularly shaped uterus have a higher risk of developing an ectopic pregnancy.
Ectopic pregnancies are not viable and need to be treated right away by a doctor. Visit your OB-GYN right away if you feel severe stomach pain following a positive pregnancy test but before the pregnancy has been officially confirmed by ultrasound. To examine you, they could use an ultrasound.
Placental Abruption
Placental abruption occurs in about 1% of pregnant women, usually during the third trimester. The placenta’s premature detachment from the uterine wall can cause severe, ongoing lower abdominal pain that only gets worse over time. If you press on your abdomen, your uterus can become rock hard, and you might hemorrhage dark, red blood without any clots.
A medical professional may decide to monitor your pregnancy in milder circumstances, though they may also decide to induce labor and have a vaginal delivery. A Caesarean section may be required in an emergency if the condition itself induces labor.
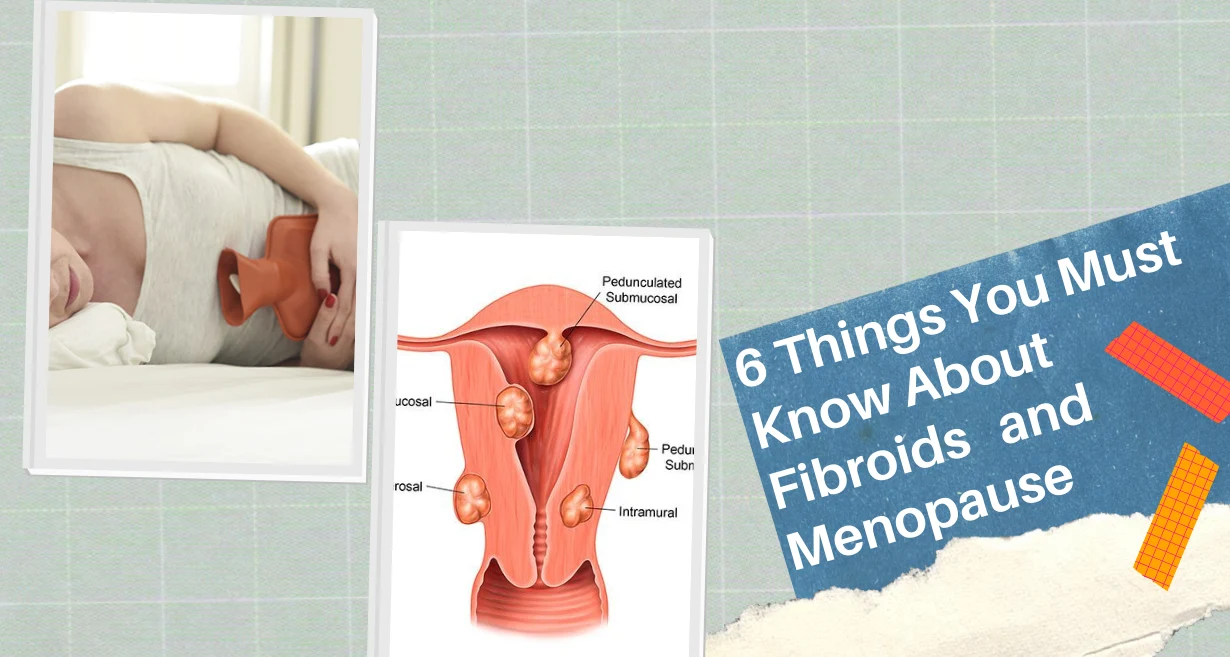
Uterine Fibroids
During the childbearing years, uterine fibroids are frequent, but pregnancy further encourages these benign growths. Pelvic pain results from them degenerating if they grow too quickly and outrun their own blood supply. Sometimes they need to be surgically removed in order to continue the pregnancy.
Uterine Rupture
Even while it happens very infrequently, it is possible for the uterus to rupture during pregnancy, particularly if you have scarring from a previous C-section or other abdominal surgery. Around the site of the trauma, you’ll experience an abrupt, excruciating, tearing abdominal or pelvic agony.
While there is no way to stop it, let your doctor know if you’ve ever suffered an injury there so they can keep an eye on your health. If discomfort starts later in the pregnancy and grows severe, call them immediately.
Preeclampsia
Preeclampsia is an often uncomfortable condition that can start any time after the 20th week of pregnancy and affects 5% to 8% of pregnant people. Symptoms include the sudden start of high blood pressure, probable kidney or liver damage, and constriction of blood arteries around the uterus (which can significantly reduce the flow of oxygen and nutrients to the baby).
A placental abruption is also more likely when preeclampsia is present. When the illness is severe, it can cause nausea, headaches, and vision problems, as well as pain in the upper right area of your abdomen. High blood pressure and unusual swelling in the hands, feet, and face are frequently people’s first signs of illness. The moment you suspect you may have preeclampsia, call a doctor.
Ovarian Torsion
In a few instances, ovarian torsion—when an ovary twists around its associated ligaments and shuts off its own blood supply—causes stomach or pelvic pain, nausea, and fever. Although it can happen at any point in the pregnancy, the early stages are when it happens most frequently. If you have ovarian cysts or have had ovulation induction, which can result in larger ovaries, you may be more at risk.
Appendicitis
Because the appendix is pushed up higher in the belly as pregnancy progresses, appendicitis might sneak up on you during this time. Though it might move, you’ll typically feel it in the bottom right portion of your abdomen. Emergency surgery is frequently required in the event of appendicitis to remove the appendix before it ruptures.
Related Blog – 15 Kegel Exercises for Pregnant Women and Their Benefits (2023)
Treatment Of Pelvic Pain During Pregnancy
The goals of treating pelvic pain during pregnancy are to reduce symptoms, provide comfort, and protect the mother and the unborn child. Here are a few methods for treating pelvic pain when pregnant:
Rest and Positioning
Avoiding activities that make the pain worse while resting might help ease discomfort. Frequent position changes and the use of supportive pillows or cushions can add to the relief. Maintaining proper posture and avoiding prolonged standing or sitting in one place is also crucial.
Physical Therapy
Managing pelvic pain during pregnancy can be effectively treated with physical therapy. In order to increase stability, promote good body mechanics, and strengthen the pelvic floor muscles, a physical therapist might offer exercises and procedures. They might also provide manual treatment, including joint mobilization or massage, to ease discomfort and increase mobility.
Maternity Support Belts
Wearing a pelvic girdle or maternity support belt might give the pelvic region stability and aid to reduce pelvic pain. These belts lessen pressure on the pelvic joints and ligaments by more evenly distributing the baby’s weight.
Heat or Cold Therapy
Putting hot or cold compresses on sore spots can make them feel better. Muscles can be soothed and blood flow can be enhanced with the use of heat therapy, such as a warm compress or hot water bottle. An ice pack or other form of cold therapy can reduce inflammation and numb the area.
Painkillers
There are some painkillers that may be used to treat pelvic pain during pregnancy. Tylenol (acetaminophen) is usually regarded as safe for use during pregnancy, but you should always talk to your doctor before taking any medications.
Transcutaneous Electrical Nerve Stimulation (TENS)
Using electrodes attached to the skin, TENS therapy stimulates the affected area with gentle electrical impulses. It can ease pelvic pain during pregnancy and assist lessen pain signals. TENS devices should only be used with a doctor’s supervision.
Prenatal Massage
Prenatal massage administered by a licensed therapist can aid in easing pain, promoting relaxation, and reducing muscle tension. In order to assure safety and suitable techniques, it’s crucial to select a massage therapist with experience in prenatal treatment.
Before beginning any treatment for pelvic discomfort during pregnancy, it’s crucial to speak with a healthcare professional. They can assess the intensity of the pain, rule out any underlying illnesses, and offer individualized recommendations for efficiently controlling the pain while taking the demands of the pregnancy into account. Pelvic pain during pregnancy can be reduced with the right treatment and management, giving women a more pleasant and enjoyable pregnancy.
Related Blog – 7 Symptoms Of Ovarian Cyst You Should Not Ignore
When To Contact The Doctor
If you have pelvic pain and have a sneaking suspicion that anything is wrong, don’t wait to call your doctor. Your doctor would much rather you call and find out there is no need for concern than not call and run the risk of a catastrophic problem.
Quickly contact your doctor if you experience any of the following signs:
- Pelvic pain that prevents you from moving or speaking
- A rise in temperature or chills
- Bleeding if any
- Terrible headache
- Dizziness
- Sudden swelling on the face, or hands and feet
- Persistent dizziness or nausea
- If you are between 28 weeks and birth, you experience fewer than 10 fetal kicks in an hour.
- Two hours of more than four contractions per hour
- Bloody, green, or watery discharge
Takeaway
Because it is a symptom of so many different illnesses, pelvic pain can be both unsettling and aggravating. In order to get the treatment you need to feel better, your doctor can assist in identifying the source of your pelvic pain. Good prenatal care is essential for the healthy growth of your unborn child as well as for the mother’s pain-free pregnancy. Having a top-notch group of obstetricians and gynecologists on your side is also beneficial, and that is what you get at Queen’s Gynaecology in Delhi. The highly qualified and competent medical staff at Queen’s Gynaecology will not only allay your fears regarding your symptoms but will also provide you with top-notch care so that you can continue to experience a pain-free and enjoyable pregnancy.
Frequently Asked Questions
The majority of the time, mild activity helps pregnant women manage pelvic pain. To get the right exercise advice catered to your condition, though, it’s crucial to speak with a medical professional or a physical therapist who specializes in prenatal care.
Warm baths, using a pregnant support belt, using heat or cold packs, maintaining excellent posture, and taking a nice nap are a few home remedies that might help. Before attempting any at-home treatments, it is, however, always advisable to speak with a healthcare professional.
The health or development of the fetus is often unaffected by pelvic pain in and of itself. To guarantee the well-being of both the mother and the unborn child, certain underlying conditions that are causing the discomfort might need to be treated or managed.
Some painkillers, such as paracetamol (Tylenol), are typically regarded as safe to use while pregnant. To ensure safety and the right dosage, it is essential to speak with a healthcare professional before taking any medicine while pregnant.
As the body returns to its pre-pregnancy state after giving birth, most women experience a decrease in pelvic pain. However, some women may have ongoing pelvic pain after giving birth, so it’s crucial to address any discomfort with a healthcare professional for a thorough assessment and the best course of action.